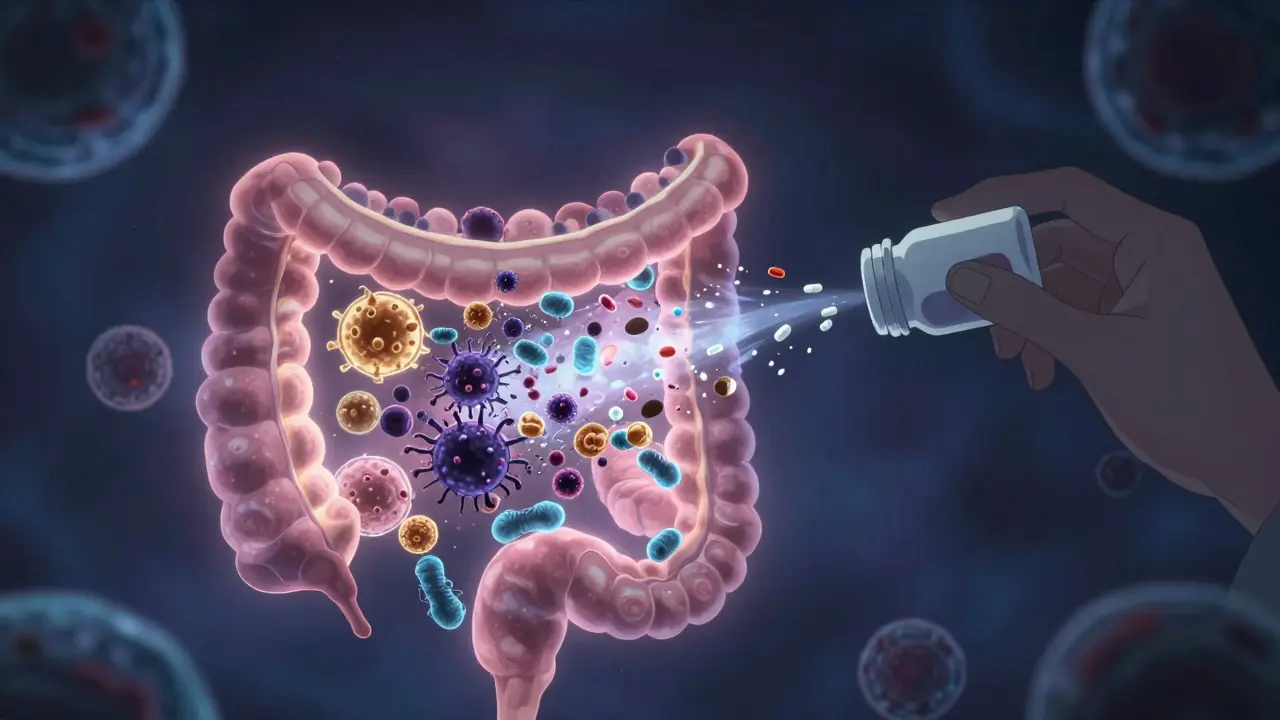
Every time you take an antibiotic, you’re not just fighting an infection-you’re changing the balance of trillions of bacteria inside your gut. Most people don’t realize that antibiotics don’t pick and choose. They wipe out both the bad bugs and the good ones. And when the good ones disappear, dangerous ones like Clostridioides difficile can take over, causing severe diarrhea, colitis, and even death. This isn’t just a hospital problem. It’s happening in homes, clinics, and doctor’s offices across the country.
Why Antibiotic Stewardship Isn’t Just a Hospital Policy
Antibiotic stewardship sounds like a bureaucratic term, but it’s really just common sense: use antibiotics only when they’re truly needed, and use them the right way when you do. The CDC defines it as measuring and improving how antibiotics are prescribed and taken. Simple, right? Yet in the U.S., nearly half of all outpatient antibiotic prescriptions for respiratory infections are unnecessary. That’s 46% of prescriptions that do more harm than good. This isn’t about being overly cautious. It’s about survival. The World Health Organization calls antimicrobial resistance one of the top 10 global public health threats. Every year in the U.S. alone, more than 2.8 million infections from antibiotic-resistant bacteria occur. Over 35,000 people die. And the biggest driver? Overuse and misuse of antibiotics. Stewardship isn’t about saying no to antibiotics. It’s about saying yes to the right antibiotic, at the right dose, for the right length of time. That’s it. When done well, it saves lives, cuts costs, and protects your gut.How Antibiotics Break Your Gut Balance
Your gut is home to trillions of bacteria-most of them helpful. They help digest food, train your immune system, and even make vitamins. Antibiotics don’t distinguish between good and bad. They hit everything. That’s why after a course of antibiotics, many people get diarrhea, bloating, or yeast infections. The real danger comes from Clostridioides difficile, or C. diff. This nasty bacterium can lie dormant in your gut until antibiotics wipe out the competition. Then it explodes. C. diff causes severe, life-threatening diarrhea. In the U.S., it leads to 223,900 infections and 12,800 deaths each year. And antibiotics are the #1 risk factor. About 1 in 5 people who take antibiotics develop C. diff. The good news? You don’t need to take antibiotics for every sniffle or sore throat. Most colds, flu, and even many sinus and ear infections are viral. Antibiotics won’t help. But too often, doctors prescribe them anyway-because patients expect them, or because it’s faster than explaining why they’re not needed.The Five Pillars of Effective Antibiotic Stewardship
Hospitals and clinics that do stewardship right follow a clear framework from the CDC. It’s not complicated:- Leadership commitment - Someone has to own it. Usually, that’s an infectious disease doctor and a clinical pharmacist working together.
- Accountability - Who’s responsible for tracking prescriptions? Someone must be named.
- Drug expertise - Pharmacists with special training in antibiotics are key. They know which drugs work, which don’t, and which are overkill.
- Action - This is where it happens: reviewing prescriptions, suggesting alternatives, shortening courses, or stopping them entirely.
- Tracking and reporting - Hospitals track how many antibiotics they give per 1,000 patient days. They also watch for C. diff rates. If one goes up, the other usually follows.
What You Can Do as a Patient
You don’t have to wait for a hospital program to protect yourself. Here’s what you can do:- Ask: “Is this really an infection that needs antibiotics?” If you have a cough, sore throat, or runny nose, ask if it’s viral. Viral infections don’t respond to antibiotics.
- Ask: “What’s the shortest effective course?” Many infections-like ear infections or sinusitis-can be treated in 5 to 7 days, not 10. Shorter courses mean less damage to your gut.
- Ask: “Is there a narrower-spectrum antibiotic?” Broad-spectrum drugs like amoxicillin-clavulanate hit everything. Narrow-spectrum ones like penicillin V target only the bugs causing the problem. Fewer side effects, less resistance.
- Don’t pressure your doctor. If they say no, don’t push. They’re not being difficult-they’re being careful.
- Don’t save leftover antibiotics. Storing old pills for “next time” is dangerous. The wrong dose, wrong bug, wrong timing-it can make things worse.
Outpatient Settings Are the Biggest Problem
Most antibiotic misuse happens outside hospitals-in doctor’s offices, urgent care centers, and pharmacies. A study found that doctors prescribed antibiotics for acute respiratory infections 46% of the time when they weren’t needed. That’s nearly 1 in 2 cases. The fix? Simple tools. One clinic put up posters in exam rooms that said: “I promise to only prescribe antibiotics when they’re truly needed.” That alone cut inappropriate prescribing by 5.6%. Another used electronic alerts that popped up when a doctor tried to prescribe amoxicillin for a viral cough. The rate dropped by 30%. Even small practices can do stewardship. The University of Nebraska’s program helps rural and critical-access hospitals with remote support. They train staff, provide checklists, and offer real-time advice. You don’t need a big hospital budget. You just need the will to do better.What’s Next? AI, Diagnostics, and Faster Decisions
The future of stewardship is getting smarter. New rapid tests can tell if an infection is bacterial or viral in under an hour. That’s huge. Right now, doctors often guess. With faster diagnostics, they can know. Some hospitals are testing AI tools that analyze patient data and suggest the best antibiotic within seconds. One pilot program improved appropriate prescribing by 15-20%. These tools don’t replace doctors-they help them make better decisions faster. The CDC’s Antimicrobial Resistance Laboratory Network is expanding across the country. It’s tracking exactly which bugs are resistant where. That means doctors can choose antibiotics that still work in their region, instead of guessing.
The Bigger Picture: Why This Matters for Everyone
Antibiotic resistance isn’t a distant threat. It’s here. And it’s personal. If you’ve ever had a surgery, a hip replacement, chemotherapy, or even a simple C-section-you’ve relied on antibiotics to keep you safe from infection. If they stop working, those procedures become deadly. The economic cost is staggering. In the U.S., inappropriate antibiotic use costs $1.1 billion a year in outpatient care alone. Hospitals save up to $1.1 billion annually just by cutting down on unnecessary prescriptions and preventing C. diff. By 2025, the CDC estimates that widespread stewardship could prevent 130,000 C. diff infections and save 10,000 lives. That’s not a guess. That’s data.Final Thought: Antibiotics Are Powerful-But Not Magic
Antibiotics saved millions of lives in the 20th century. But they’re not a cure-all. They’re a tool. And like any tool, they wear out if you use them carelessly. Protecting your gut health isn’t just about probiotics and yogurt. It’s about being smart about when-and whether-you take antibiotics. Every unnecessary pill you avoid is one less chance for resistance to grow. One less chance for C. diff to take hold. One less chance for the next generation to face a world where simple infections become deadly again. You don’t need to be a doctor to be part of the solution. Just ask questions. Say no when it’s not needed. And remember: sometimes, the best medicine is no medicine at all.Do antibiotics always kill good bacteria in the gut?
Yes, all antibiotics affect the gut microbiome to some degree. Broad-spectrum antibiotics like amoxicillin, ciprofloxacin, and clindamycin hit a wide range of bacteria, including the beneficial ones. Even narrow-spectrum antibiotics can disrupt the balance. The extent depends on the drug, dose, and length of treatment. Shorter courses and targeted antibiotics cause less damage.
Can probiotics prevent C. diff after antibiotics?
Some studies show certain probiotics-like Saccharomyces boulardii and specific Lactobacillus strains-may reduce the risk of C. diff by about 60% in high-risk patients. But they’re not a guarantee. The best protection is avoiding unnecessary antibiotics in the first place. Probiotics help, but they can’t undo the damage of a 10-day course of clindamycin.
Are natural remedies a good alternative to antibiotics?
For viral infections like colds or flu, yes-rest, fluids, and time are the best remedies. But for confirmed bacterial infections like strep throat, urinary tract infections, or pneumonia, natural remedies won’t work. Delaying antibiotics in these cases can lead to serious complications. Don’t replace antibiotics with honey or garlic when you need a real drug.
Why do doctors still prescribe antibiotics when they’re not needed?
Pressure from patients is a big reason. Many people believe antibiotics cure all infections. Others are afraid of complications or just want to feel better fast. Time constraints also play a role-explaining why antibiotics won’t help takes longer than writing a prescription. Stewardship programs help by giving doctors tools and support to say no confidently.
Is antibiotic resistance getting worse?
Yes, and it’s accelerating. The CDC reports that resistant infections are rising in hospitals and communities. Some bacteria are now resistant to nearly all available drugs. New antibiotics aren’t being developed fast enough. That’s why stewardship is critical-it preserves what we still have.
Can I take antibiotics for a sinus infection?
Most sinus infections are viral and clear up on their own in 10-14 days. Antibiotics are only needed if symptoms last longer than 10 days, get worse after initial improvement, or include high fever and thick, colored discharge for more than 3 days. Many doctors still prescribe them too early-but you can ask for a wait-and-see approach.
What happens if I stop antibiotics early?
You should never stop antibiotics without talking to your doctor. But the old rule-“always finish the full course”-is being reevaluated. For some infections, like strep throat or uncomplicated UTIs, shorter courses are just as effective and cause less resistance. The key is taking the right dose for the right time, not just taking it until the bottle is empty.




Reviews
lol i just took amoxicillin last week for a sore throat that turned out to be viral. my gut has been weird since. guess i learned the hard way.
YES. This is so important. I used to beg my doctor for antibiotics every time I felt under the weather. Now I ask, "Is this viral?" and I actually wait it out. My digestion has never been better. Small changes = huge impact. 🙌
I work in a clinic and see this every day. Patients come in expecting a script. We spend 10 minutes explaining why they don’t need it. Some get mad. Others leave grateful. It’s exhausting but worth it. Thank you for writing this.
It is, indeed, a matter of profound public health consequence that the collective unconscious of modern society has come to equate pharmaceutical intervention with therapeutic efficacy-regardless of etiology. The gut microbiome, that intricate and ancient symphony of microbial life, is not merely a passive organ but a dynamic, co-evolved ecosystem whose disruption precipitates cascading physiological and immunological consequences. To prescribe antibiotics indiscriminately is not merely medical negligence; it is an act of ecological vandalism upon the very foundation of human biological integrity. The rise of C. diff, the normalization of antibiotic resistance, the erosion of therapeutic efficacy-these are not abstract statistics. They are the inevitable crescendo of a century of biological arrogance. We must, with solemn urgency, recalibrate our relationship with these molecules-not as panaceas, but as precision instruments, wielded only by the wise.
While the article presents a compelling narrative grounded in empirical data, one must interrogate the underlying epistemological framework that privileges institutional authority over individual autonomy. The CDC’s "five pillars," though seemingly rational, are, in essence, bureaucratic mechanisms designed to standardize medical behavior under the guise of stewardship. Who defines "necessary"? Who holds the power to determine the threshold of "viral" versus "bacterial"? The answer, of course, lies in the institutional apparatus-not in the lived experience of the patient. One wonders: is this stewardship, or is it medical paternalism dressed in the language of science?
Ok but like… have you seen the CDC’s new AI tool that predicts resistance patterns? 😱 It’s wild. Like, you type in symptoms and it tells you which antibiotic works in your county. 2025 is gonna be insane. Also, I took a probiotic after my last round and now I have the gut of a 12-year-old. 🤫✨ #antibioticawareness #guthealth
There’s something poetic about how we’ve weaponized biology against itself. We create antibiotics to kill the bad, but in doing so, we starve the good-the trillions of tiny allies that have coexisted with us since before we were human. It’s like burning down your house to get rid of one cockroach. And then we wonder why we’re sick again. The real miracle isn’t the drug-it’s the microbiome. And we’re treating it like trash. Maybe the next frontier isn’t new antibiotics… but rewilding our insides. Probiotics help, sure. But what if we started asking: what did we do to make our guts so fragile in the first place?
People take antibiotics like candy. They don't know what they're doing. This is why the world is ending. God gave us bodies to heal. Medicine is for the weak. Stop trusting doctors. Let your body fight. It's the natural way.
Let’s be real-antibiotics are just the tip of the iceberg. Big Pharma and the CDC are in bed together. They want you dependent. They want you scared of every sniffle. They profit from your fear. The real reason they push stewardship? So they can control which drugs you get and when. And what about the glyphosate in your food? The EMFs? The vaccines? All of it’s connected. Your gut is a sensor. And they’re poisoning it on purpose. Wake up.
i stopped asking for antibiotics last year and my stomach stopped acting like a dumpster fire. also my doctor was like "wow you’re actually smart" lmao