Have you ever taken a medication that didn’t work-or made you feel worse? You’re not alone. For many people, the same dose that helps one person causes side effects in another. The reason often lies not in the drug itself, but in your genes. This is where pharmacogenomics comes in: the science of how your DNA shapes how your body handles medicine.
Why Your Genes Matter When You Take a Pill
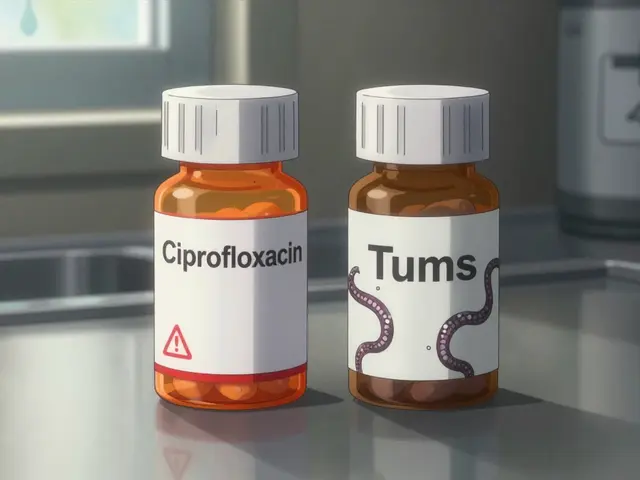
Most people think of drugs like one-size-fits-all tools. Take the same pill, get the same result. But that’s not how biology works. Your body processes medications through enzymes-proteins that break down, activate, or move drugs around. And those enzymes? They’re made by genes. Small differences in those genes can turn you into a fast, slow, or even non-responsive metabolizer of certain drugs. Take CYP2D6, one of the most important drug-metabolizing enzymes. It handles about 25% of all commonly prescribed medications, including antidepressants like fluoxetine, beta-blockers like metoprolol, and painkillers like codeine. If you have two copies of a variant that makes this enzyme work too well, you might turn codeine into morphine too quickly-and risk overdose. If your enzyme barely works at all, codeine won’t help your pain. This isn’t rare. Around 1 in 10 people of European descent are poor metabolizers of CYP2D6. For others, it’s ultra-rapid. And no two people are the same.How Pharmacogenomics Changes Treatment
Traditional prescribing is guesswork. Doctors start with a standard dose, watch for side effects, adjust, repeat. It’s inefficient-and dangerous. In the U.S. alone, over 1.3 million emergency visits each year are caused by adverse drug reactions. About 70% of those could be prevented with genetic testing. Pharmacogenomics flips the script. Instead of trial and error, doctors use your genetic profile to pick the right drug and dose from the start. For example:- People with a specific variant in CYP2C19 don’t respond well to clopidogrel (Plavix), a blood thinner used after heart attacks. Without testing, they’re at higher risk of another heart event. Testing identifies these patients so they can switch to a different drug.
- Patients with TPMT deficiency can’t process thiopurines (used in leukemia and autoimmune diseases). Giving them the standard dose can cause fatal bone marrow suppression. Genetic screening before treatment prevents this.
- For warfarin, the classic blood thinner, combining CYP2C9 and VKORC1 gene results helps doctors hit the right dose faster-cutting bleeding risks by 31% in the first month.
Who Benefits Most?
Not everyone needs genetic testing before taking a pill. But for certain groups, it’s a game-changer:- People with treatment-resistant depression: Up to 60% of patients don’t respond to first-line antidepressants. Genetic testing can explain why-and point to better options like bupropion or venlafaxine.
- Cancer patients: Drugs like 5-fluorouracil (5-FU) can be deadly if you have a DPYD gene mutation. Testing before treatment saves lives.
- Patients on multiple medications: Polypharmacy increases the risk of harmful interactions. Pharmacogenomics helps untangle which drugs are safe to combine.
- Older adults: As liver and kidney function decline with age, metabolism slows. Genetic data helps fine-tune doses to avoid toxicity.
What Tests Are Used?
Most clinical tests look at 50 to 100 genes linked to drug response. The most common include:- CYP2D6: Metabolizes antidepressants, opioids, beta-blockers
- CYP2C19: Affects clopidogrel, proton pump inhibitors, some antidepressants
- CYP2C9 and VKORC1: Critical for warfarin dosing
- TPMT and DPYD: Prevent life-threatening toxicity from chemotherapy drugs
- SLCO1B1: Influences statin side effects-people with certain variants have a 4.5x higher risk of muscle damage from simvastatin
Limitations and Challenges
Pharmacogenomics isn’t magic. It doesn’t work for every drug. Right now, only about 12% of FDA-approved drug labels include actionable genetic information. Many medications are broken down by multiple pathways, so one gene doesn’t tell the whole story. Cost is another barrier. A full panel can run $250-$500. While insurance coverage is improving-87% of Medicare Advantage plans now cover at least one PGx test-many still require prior authorization. Some patients wait over two weeks just to get approval. And there’s a big equity gap. Over 90% of pharmacogenomics research has been done in people of European descent. That means the data we use to interpret results doesn’t reflect the genetic diversity of the global population. A variant common in African, Asian, or Indigenous populations might be overlooked. This isn’t just a scientific flaw-it’s a health justice issue.
What’s Next?
The future is pre-emptive testing. Imagine getting your pharmacogenomic profile done once, as a teen, and having it stored in your medical record for life. Every time a doctor prescribes a new drug, the system automatically flags if your genes suggest a risk or benefit. The UK’s 100,000 Genomes Project showed that embedding PGx into routine care reduced medication-related hospital admissions by 31%. The NIH’s $190 million IGNITE Network is now pushing for broader implementation across diverse populations. By 2030, experts predict routine PGx screening at age 18 will become standard. Meanwhile, programs like the VA’s Medication Safety initiative have already tested over 100,000 veterans. Results? 22% fewer hospitalizations. That’s not theory. That’s real-world impact.How to Get Started
If you’re on multiple medications, have had bad reactions, or your depression or pain hasn’t responded to treatment, ask your doctor about pharmacogenomic testing. You don’t need to wait for a specialist. Many primary care providers now work with pharmacists or genetic counselors who can help interpret results. You can also get limited PGx data through direct-to-consumer tests like 23andMe, which reports on seven medications. But these aren’t diagnostic. For clinical decisions, always use a test ordered by a healthcare provider and interpreted by a trained professional. The key is to act on the results. A test without action is just data. But when paired with the right guidance, it can prevent hospital stays, reduce suffering, and finally get you the right treatment.Pharmacogenomics isn’t the future of medicine. It’s already here. And for millions of people who’ve been let down by trial-and-error prescribing, it’s the answer they’ve been waiting for.





Reviews
Let’s be real-this whole pharmacogenomics thing is just corporate medicine’s way of selling more tests. You think your CYP2D6 status is gonna save you? Nah. It’s just another line item on your insurance bill while Big Pharma keeps pricing drugs like they’re selling gold-plated aspirin. And don’t get me started on the ‘one-size-fits-all’ myth-everyone knows doctors are just guessing anyway. This isn’t science. It’s marketing with a DNA swab.
And don’t even mention equity. Of course 90% of the data is from white people. Who do you think funds these studies? Silicon Valley VCs who’ve never met a person of color. This isn’t precision medicine. It’s precision exclusion.
Stop pretending this is revolutionary. It’s just another way to make you feel like your body is broken until you pay for the ‘fix’.
Meanwhile, your grandma’s still on warfarin because her doctor doesn’t have time to decode your genome. Real medicine doesn’t need a 27-gene panel. It needs empathy. And a damn good pharmacist.
And yes, I’ve read the JAMA paper. It’s funded by a company that sells these tests. Surprise, surprise.
man i just read this and i’m crying a little. i’ve been on 7 different antidepressants and none of them worked. i thought it was me. like maybe i was just too broken to heal. turns out my CYP2C19 is trash and my body just ate up the meds like they were candy. if i’d known this 5 years ago…
my doc never mentioned testing. said it was ‘experimental.’ but now i see it’s just not covered. i’m gonna push for it next visit. thank you for writing this. you made me feel less alone.
While the scientific underpinnings of pharmacogenomics are undeniably compelling the implementation remains fraught with systemic inefficiencies and ethical lacunae. The assertion that genetic profiling constitutes a paradigm shift in clinical practice is predicated upon the assumption of equitable access-a condition presently unmet. Moreover the commercialization of genetic data introduces profound privacy concerns which are insufficiently addressed by current regulatory frameworks. One must interrogate whether the reduction of human physiology to a genomic algorithm is truly therapeutic or merely technocratic.
It is imperative that we prioritize robust longitudinal studies across diverse populations before institutionalizing these protocols. Otherwise we risk entrenching health disparities under the veneer of innovation.
Bro this is wild. I had no idea my body was basically a different species from everyone else’s when it comes to meds.
My doc just gave me the same painkiller as my buddy and I ended up in the ER. He was fine. I was sweating and dizzy. Turns out I’m a CYP2D6 ultra-rapid metabolizer 😅
Got tested last month. Best $300 I ever spent. Now my doctor actually knows what he’s doing. I’m not a guinea pig anymore.
Also 23andMe told me I’m bad with statins. So I switched to ezetimibe and my muscles don’t feel like they’re made of cement anymore. 🙌
Everyone should get this done if they’re on more than 2 prescriptions. It’s not sci-fi. It’s just… common sense.
Oh wow. Another woke science article pretending genetics is a magic bullet. Let me guess-you think this will fix opioid addiction? Or that your CYP2D6 status makes you immune to poor lifestyle choices? You’re not special. You’re just a statistic with a swab.
People die from bad meds because they don’t take them right. Not because their genes are ‘wrong.’
And don’t give me that ‘equity’ nonsense. If you can’t afford to get tested, maybe you shouldn’t be on 12 medications. Stop blaming the system. Take responsibility.
This is just another way for the medical-industrial complex to profit off anxiety. I’ve seen too many patients get scared into buying useless tests. Your genes don’t make you fragile. Your mindset does.
Bro this is next level. In India we’re still stuck with doctors prescribing paracetamol for everything because they don’t even know what CYP enzymes are. But I’ve seen this work in Bangalore’s private clinics-people on clopidogrel who were having mini-strokes? Switched after testing. No more hospital trips.
And yeah, the data gap? Massive. We’ve got variants in South Asian populations that don’t even show up in the databases. Like that one CYP2C19 splice variant that’s common in Kerala but labeled ‘unknown significance’ in the US guidelines.
But here’s the thing-it’s not about replacing doctors. It’s about giving them a flashlight in the dark. I’ve seen docs cry when they realize they’ve been dosing someone wrong for years. This ain’t magic. It’s justice with a lab report.
Also, I just got my 23andMe results. Turns out I’m a slow metabolizer for SSRIs. Now I know why I felt like a zombie on sertraline. 😅
There’s something deeply human about this. We’ve spent centuries treating people like machines with broken parts. But here-finally-we’re starting to see that bodies aren’t standardized. Each of us is a unique symphony of enzymes, genes, and history.
And yes, cost and access are problems. But that doesn’t mean the science is flawed. It means our systems are. We can fix the systems. We can’t fix biology.
I’ve worked with patients who’ve spent years in depression hell. One test changed their life. Not because it was perfect. But because it gave them back agency. They weren’t ‘failing treatment.’ Their body was just speaking a different language.
Maybe the real revolution isn’t the test. It’s the humility it forces us to have. We don’t know everything. And that’s okay.
Let’s not make this about profit. Let’s make it about dignity.
How quaint. A 2022 JAMA study shows a 27% increase in remission rates? How many of those patients were on placebo? How many were simply receiving more attentive care because they were enrolled in a ‘genetic’ program? Confirmation bias dressed in sequencing data.
And let’s not pretend this isn’t just a glorified version of blood type matching from the 1950s. We’ve known for decades that metabolism varies. This is just rebranding with a fancy panel.
Also, the VA’s ‘22% fewer hospitalizations’? Correlation ≠ causation. Maybe they just improved medication reconciliation protocols. Or hired more pharmacists. Or stopped prescribing opioids like candy.
Don’t mistake novelty for necessity. The real innovation is still the doctor-patient relationship. Not a cheek swab.