Daily Fluid Goal Calculator
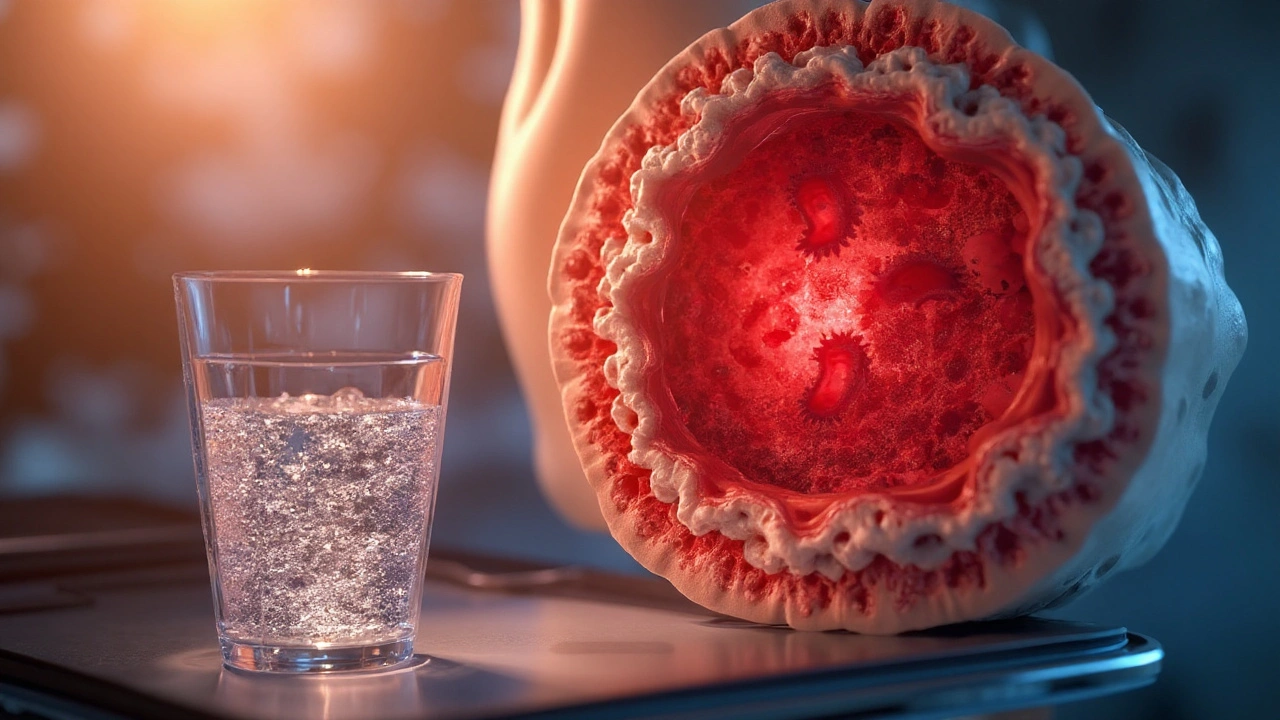
Bone Marrow Disorders are a group of medical conditions that impair the bone marrow’s ability to produce healthy blood cells. They include leukemia, aplastic anemia, myelodysplastic syndromes and severe forms of anemia. When the marrow can’t keep up, the body’s oxygen‑carrying capacity, immune defense, and clotting ability all suffer.
TL;DR
- Bone marrow disorders reduce blood volume and increase dehydration risk.
- Proper hydration supports circulation, kidney function, and treatment tolerance.
- Fluid needs differ between leukemia, aplastic anemia, and myelodysplastic syndromes.
- Electrolyte‑balanced drinks are often better than plain water alone.
- Monitor urine color, weight, and symptoms; seek care if you feel dizzy or faint.
Understanding the Main Bone Marrow Disorders
Leukemia is a cancer of the blood‑forming tissue that causes uncontrolled proliferation of abnormal white blood cells. It often leads to anemia, bleeding, and frequent infections.
Aplastic Anemia is a rare condition where the marrow stops producing enough red cells, white cells, and platelets, leaving patients extremely vulnerable to fatigue and bleeding.
Myelodysplastic Syndromes (MDS) are a collection of disorders where the marrow produces defective blood cells that die early, sometimes progressing to acute leukemia.
All three share a common thread: reduced functional blood volume and a heightened need for supportive care, especially fluid balance.
Why Hydration Is More Than Just Drinking Water
Hydration maintains extracellular fluid volume, which is essential for delivering oxygen and nutrients to tissues. In bone marrow disorders, the body’s ability to regulate fluid shifts is compromised because:
- Low red blood cell counts reduce oxygen delivery, prompting the heart to work harder and increasing sweat loss.
- Chemotherapy and immunosuppressive therapy often cause nausea, vomiting, or diarrhoea, accelerating fluid loss.
- Chronic anemia can cause renal hypoperfusion, impairing the kidneys’ capacity to concentrate urine.
These mechanisms create a perfect storm where even mild dehydration can trigger dizziness, kidney injury, or worsen treatment side‑effects.
How Dehydration Impacts Specific Disorders
Each disorder reacts differently to fluid deficits:
- Leukemia: Rapidly dividing leukemic cells consume glucose and produce metabolic waste. Adequate hydration helps kidneys flush out toxins, lowering the risk of tumor lysis syndrome.
- Aplastic Anemia: With already low platelet counts, dehydration thickens blood, increasing clot‑formation risk and making bleeding episodes harder to control.
- MDS: The fragile, poorly formed red cells are prone to hemolysis; dehydration worsens hemolytic anemia by raising blood viscosity.
In all cases, good fluid balance reduces the load on the heart, eases breathing, and supports the effectiveness of transfusions and stem‑cell grafts.

Practical Hydration Guidelines for Patients
General recommendations for adults are 2.7L (women) to 3.7L (men) of total water per day, but patients with bone marrow disorders often need more. Follow these steps:
- Start the day with 250ml of electrolyte‑rich beverage (e.g., oral rehydration solution). This jump‑starts plasma volume.
- Sip 150‑200ml every hour while awake. Set a timer or use a water‑tracking app.
- Include foods with high water content: cucumber, watermelon, broth‑based soups, and citrus fruits.
- Avoid excess caffeine and alcohol; they act as diuretics.
- During chemotherapy cycles, increase intake by an extra 500ml per day to offset nausea‑related losses.
Monitor urine color: pale straw is ideal; dark amber signals the need to drink more.
Electrolyte Management
Plain water dilutes sodium, potassium, and magnesium-key electrolytes that keep nerves and muscles functioning. For patients on diuretics or with vomiting, add a pinch of sea salt (≈0.5g) or use commercial oral rehydration salts (ORS) that provide a balanced 90mmol/L sodium and 20mmol/L potassium profile.
When kidney function is reduced (common in advanced MDS), discuss ORS dosing with a nephrologist to avoid hypernatremia.
Comparison of Hydration Needs Across Disorders
| Disorder | Typical Fluid Loss (ml/day) | Recommended Intake (ml/day) | Key Risks of Dehydration |
|---|---|---|---|
| Leukemia (treated) | ≈800 (from chemo‑induced vomiting) | ≈3500-4000 | Tumor lysis, renal failure |
| Aplastic Anemia | ≈500 (baseline) | ≈3000-3500 | Increased blood viscosity, bleeding |
| Myelodysplastic Syndromes | ≈600 (from chronic anemia) | ≈3200-3800 | Hemolysis, cardiovascular strain |
These figures are averages; individual needs may vary. Always adjust based on weight, activity, and physician advice.
Related Concepts and How They Connect
Understanding the broader picture helps you stay proactive:
- Bone Marrow Biopsy - the gold‑standard diagnostic tool; results guide fluid‑management strategies during transplant preparation.
- Stem Cell Transplant - often the curative option; patients must be eu‑volemic (properly hydrated) to tolerate conditioning regimens.
- Nutrition - adequate protein and iron support erythropoiesis; dehydration hampers nutrient absorption.
- Infection Risk - low white‑cell counts combined with dehydration impair mucosal barriers, raising infection chances.
By linking hydration to these topics, you can see why fluid balance is a cornerstone of overall care.
When to Seek Professional Help
Even with diligent drinking, certain signs demand immediate attention:
- Persistent dizziness or fainting.
- Rapid weight loss (>2kg in 48hours).
- Sudden drop in urine output (<400ml/day).
- Confusion, slurred speech, or seizures - possible electrolyte imbalance.
Contact your hematologist or go to the emergency department if any of these appear.

Frequently Asked Questions
How much water should a leukemia patient drink during chemotherapy?
Aim for at least 3.5L of fluids daily, split between water, broth, and electrolyte‑rich drinks. Increase by 500ml on days when nausea or vomiting occurs.
Can I rely solely on coffee for my daily fluid intake?
No. Coffee is a mild diuretic and can worsen dehydration, especially when blood counts are low. Limit coffee to one cup and balance it with water or ORS.
Is it safe to add salt to my water if I have high blood pressure?
Consult your doctor first. For most bone‑marrow patients, a modest salt addition (½g) helps retain fluids, but if you have hypertension, a low‑sodium ORS formulation may be better.
What signs tell me I’m dehydrated enough to stop drinking?
When urine turns light yellow, you’re likely well‑hydrated. If you notice swelling, shortness of breath, or a rapid weight gain, you may be over‑hydrating and should seek advice.
Do oral rehydration solutions interfere with my medication schedule?
Generally they don’t, but some antibiotics absorb better on an empty stomach. Take the ORS at least 30minutes apart from such meds unless your physician advises otherwise.



Reviews
Hydration isn't just about water. It's about electrolyte balance, renal perfusion, and preventing tumor lysis syndrome. Plain H2O alone can dilute sodium and trigger hyponatremia in chemo patients. ORS isn't optional-it's medical necessity.
Man, I wish I'd known this when my uncle was going through MDS. We were just giving him Gatorade and calling it good. Turns out, the sodium-to-potassium ratio in ORS matters way more than the sugar content. That little salt pinch? Game changer. His kidneys stopped screaming after we switched.
Good breakdown. I'd add that hydration also helps with mucosal integrity-especially important when WBC counts are low. Dry mouth isn't just uncomfortable; it's a portal for infection. Sipping constantly isn't just advice-it's armor.
This is the kind of info that should be handed out at every oncology appointment. Not just posted online. My sister’s nurse never mentioned urine color as a metric-we were guessing for weeks.
Oh, so now we're treating bone marrow disorders like they're marathon runners? Let me guess-next you'll be recommending IV hydration before chemotherapy so they can 'perform better.' Pathetic. This isn't wellness culture. This is medicine. And medicine doesn't need your coconut water and mindfulness affirmations.
Interesting... in India, we've long used nimbu pani with salt and jaggery for dehydration-it's not just tradition, it's science. The natural potassium from jaggery, sodium from salt, glucose from sugar-it's a perfect ORS substitute. Why reinvent the wheel when Ayurveda already nailed it?
Wait so you're telling me I'm not supposed to chug beer after chemo because it dehydrates me but I can drink some fancy electrolyte juice that costs 8 bucks a bottle and my insurance won't cover it but my cousin in Arizona says it's a scam and the FDA is hiding the truth about hydration and cancer and I'm supposed to believe this because some guy wrote a blog with a table and I'm supposed to trust this because he used the word 'extracellular' and I'm just supposed to shut up and sip water like a good little patient like they did in the 90s when nobody knew anything and now we have AI that tells us what to drink and I'm just supposed to believe it because it's written in bold and it has a table and I'm not allowed to question it because I'm not a doctor and I'm just a person with a bone marrow disorder trying to stay alive and not die from dehydration or kidney failure or whatever the hell is going on
Who funded this? Pharma? The ORS industry? Because the real issue is that chemotherapy protocols are designed to destroy the body, not support it. Hydration is just a band-aid for a system that's broken. They don't want you to heal-they want you to keep coming back for more rounds. Drink all you want. It won't change the fact that your marrow is being poisoned.
Biggest thing I learned after my transplant: hydration isn't about volume, it's about consistency. Sipping every hour beats chugging two liters at once. Your body can't absorb it all anyway. And yes, the urine color thing works-pale straw = good. Dark apple juice = panic mode.
Western medicine always overcomplicates everything. In our villages, we drink warm water with crushed tulsi leaves and a pinch of rock salt. No lab tests. No tables. No 3800ml calculations. Just nature. And yet, our people live longer, healthier lives. Why? Because we don't treat the body like a broken machine. We treat it like a temple.
Hydration my ass. You think drinking water fixes cancer? You think a table with numbers makes you smarter than the doctors who actually treat this stuff? I've seen patients die because they listened to some Reddit post instead of their oncologist. This isn't self-help. This is dangerous.
It's not just about the kidneys or the blood viscosity. It's about dignity. When you're too dehydrated to stand, you can't shower. You can't hold your child. You can't read a book. Hydration isn't medical-it's human. And we treat it like an afterthought.
Thank you for this. I've been sharing this with my support group in Delhi. One woman switched from bottled water to homemade ORS and her hemoglobin improved slightly. Not a cure, but a small win. Small wins matter.
Let's be honest-this is just another way for the medical-industrial complex to sell you more products. ORS packets cost $3. Water costs $0.01. Why are we being sold this as a necessity? Who benefits? Not the patient.
My mom had aplastic anemia. We didn't know any of this. We just gave her water and hoped. She passed two months after diagnosis. If we'd known about the viscosity risk, maybe... maybe she'd have had more time. Thank you for writing this. I'm printing it out and giving it to every family I know going through this.
Wow. You really think people with leukemia are gonna sip 200ml every hour? Like, do you know what chemo feels like? You think nausea is a suggestion? 'Set a timer'-yeah, right. My cousin threw up twice in five minutes. What was she supposed to do? Drink more? Try again? You're not helping. You're just making people feel guilty for being sick.
One thing no one talks about: hydration helps with mental clarity. When you're dehydrated, your brain fog gets worse. And when you're already battling fatigue and fear, that fog feels like a wall. Sipping water isn't just physical-it's emotional armor.
It's not just about drinking-it's about listening to your body. I started noticing I felt worse after drinking cold water during chemo. Switched to room temp. Felt like a new person. Sometimes the simplest things work best.
What about patients with heart failure? Can they safely drink 3.5L a day? This advice seems one-size-fits-all. What's the evidence for fluid overload risk in MDS patients with cardiac compromise?
Oh, so now we're giving medical advice to cancer patients based on a blog post with a table? That's rich. I've been in oncology for 17 years. I've seen patients die because they followed 'hydration tips' from strangers online instead of their nephrologist. You think you're helping? You're just creating a false sense of control. Real medicine doesn't come from bullet points. It comes from labs, from monitoring, from professionals who've spent decades learning this stuff. You're not a doctor. You're not even a nurse. You're just someone who read a Wikipedia page and thought they were smart enough to fix a system you don't understand. And now you're telling people to drink 3.8 liters a day? What if they have renal failure? What if they have fluid retention? What if they're on dialysis? You didn't mention that. Because you didn't think about it. You just wanted to feel like the hero of some Reddit thread. You're not helping. You're endangering people. And you have no idea how dangerous that is.