Thyroid storm isn’t just a bad day with a fast heartbeat. It’s a full-body meltdown triggered by unchecked hyperthyroidism, where your metabolism goes into overdrive so fast that organs start failing. This isn’t a condition you can wait out or treat at home. If you or someone you know has untreated Graves’ disease and suddenly develops a fever over 104°F, a heart rate above 140 beats per minute, confusion, or vomiting, this is a medical emergency. Without immediate ICU care, death is likely. Even with treatment, 8 to 25% of patients don’t survive. But if you act fast-within six hours-the chance of survival jumps to 75% or higher.
What Exactly Happens in a Thyroid Storm?
Thyroid storm is the extreme end of hyperthyroidism. Normally, your thyroid gland makes just enough thyroid hormone to keep your body running smoothly. In hyperthyroidism, it makes too much. In thyroid storm, that overproduction explodes. Free T3 and T4 levels can be three to five times above normal. These hormones flood every cell in your body, forcing them to work at warp speed. Your heart pounds. Your temperature spikes. Your brain gets foggy. Your liver struggles. Your gut shuts down.
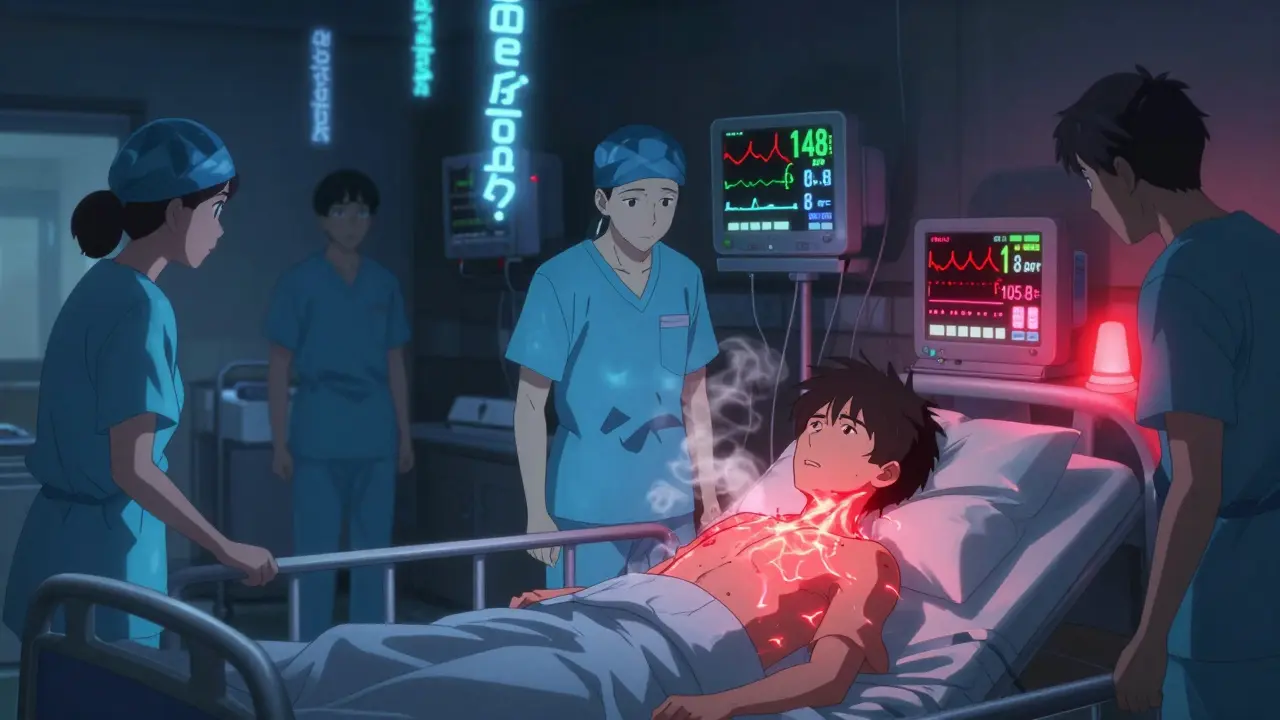
This isn’t gradual. It happens in hours. Someone with well-controlled Graves’ disease might feel fine one day, then wake up the next with a fever, shaking hands, and confusion after a bad infection or skipping their meds. The Japan Thyroid Association’s diagnostic criteria are clear: you need confirmed high thyroid hormone levels plus at least one neurological symptom (like delirium or coma) and one other major sign-fever, tachycardia, heart failure, or GI issues. Or, you can have three out of these four: fever, GI symptoms, heart failure, or tachycardia. A heart rate over 140 bpm? That’s not just anxiety. A temperature of 105.8°F? That’s a red alert.
What Triggers This Crisis?
Thyroid storm doesn’t appear out of nowhere. It’s triggered by stress on an already overactive system. In 60 to 70% of cases, it’s caused by untreated or poorly managed hyperthyroidism-often because someone stopped taking their medication. Infection is the second most common trigger, especially pneumonia or the flu. Surgery, even something routine like a tooth extraction, can set it off if thyroid levels aren’t controlled first. Trauma, including a direct blow to the neck, has been documented as a cause. Emotional shock, stroke, heart failure, and diabetic ketoacidosis are also known triggers.
Pregnancy and the postpartum period carry a higher risk. About 1 to 2% of cases are triggered by radioactive iodine treatment for Graves’ disease, sometimes weeks after the procedure. That’s why patients are warned to monitor symptoms closely after treatment. The key takeaway: if you have hyperthyroidism, any major physical or emotional stressor could be the spark. Never ignore new symptoms, even if you think you’re "on top of your condition."
How Do Doctors Diagnose It?
There’s no single blood test that says "thyroid storm." Diagnosis relies on clinical signs, lab results, and scoring systems. The Burch-Wartofsky Point Scale is the most widely used tool. It assigns points for fever, heart rate, mental status, GI symptoms, and heart failure. A score above 45 is diagnostic. A score of 25 to 44 suggests impending storm. Below 25? Unlikely.
Lab work is critical. Doctors check free T4 and free T3-both will be sky-high. TSH will be near zero. Liver enzymes and bilirubin often rise, indicating stress on the liver. A complete blood count may show high white blood cells from infection or stress. Electrolytes are often imbalanced. An arterial blood gas can reveal respiratory alkalosis from hyperventilation. An ECG will show sinus tachycardia, sometimes with atrial fibrillation. Chest X-rays may reveal heart enlargement or fluid buildup.
It’s easy to mistake thyroid storm for sepsis, a heart attack, or a panic attack. But the combination of extreme fever, tachycardia, altered mental status, and GI symptoms in someone with known hyperthyroidism is a red flag no ICU team misses.

ICU Treatment: The Race Against Time
Time is the biggest factor in survival. Every hour counts. Treatment starts within one to two hours of suspicion. It’s not one drug-it’s a layered assault on multiple fronts.
First: Block hormone production. Methimazole (60-80 mg loading dose) or propylthiouracil (PTU, 600-1000 mg) is given immediately. PTU is preferred in storm because it also blocks the conversion of T4 to the more potent T3. These drugs don’t work instantly-they take hours to reduce hormone output.
Second: Stop hormone release. One hour after antithyroid drugs, potassium iodide (500 mg every 6 hours) or sodium iodide is given. This floods the thyroid with iodine, shutting down further hormone release. It’s like slamming the brakes on a runaway train.
Third: Calm the body down. Beta-blockers, especially propranolol, are essential. They don’t lower hormone levels, but they block the effects. A typical dose is 60-80 mg every 4-6 hours, or IV doses of 1-2 mg every 5 minutes if heart rate is over 140. This brings down the pounding heart, reduces tremors, and calms anxiety. Acetaminophen is used for fever. Never use aspirin or NSAIDs-they can displace thyroid hormones from proteins and make things worse.
Fourth: Protect the adrenal glands. High-dose hydrocortisone (100 mg IV every 8 hours) is given to prevent adrenal crisis, which can happen when the body is under extreme stress. Corticosteroids also help block T4-to-T3 conversion.
Fifth: Support the body. Fluids are critical-many patients are dehydrated from sweating and diarrhea. Two to three liters of IV saline are common. Oxygen, continuous cardiac monitoring, and temperature control (cooling blankets, ice packs) are routine. If the patient is confused or unconscious, they may need intubation and mechanical ventilation. Vasopressors like norepinephrine are used if blood pressure drops.
For the most severe cases that don’t respond, plasmapheresis can remove thyroid hormones directly from the blood. Studies show a 78% success rate in refractory cases. Experimental treatments like IL-6 inhibitors are being tested but aren’t standard yet.
What Happens After the Crisis?
Survivors don’t walk out of the ICU cured. The underlying hyperthyroidism must be permanently addressed. In 85% of cases, patients end up needing lifelong thyroid hormone replacement after radioactive iodine therapy or thyroid surgery. The remaining 15% may achieve remission with long-term antithyroid drugs, but relapse is common without strict follow-up.
Neurological recovery follows a pattern: agitation fades in 24 to 48 hours. Confusion improves over 72 hours. Full mental clarity usually returns in 7 to 14 days. But the physical toll is heavy. In one study of 37 patients, 68% needed a breathing machine for an average of five days. 41% required drugs to keep their blood pressure up. The average ICU stay was almost eight days. Total hospitalization lasted over two weeks.
Long-term survival depends on adherence. Patients who skip follow-up appointments or stop their meds have a 25 to 30% chance of another storm. Those who stick with their endocrinologist have only a 2 to 3% recurrence risk.
Who’s Most at Risk?
While thyroid storm is rare-only 0.2 cases per 100,000 people per year-it hits certain groups harder. Elderly patients have a 30% mortality rate. Those with pre-existing heart disease are 2.3 times more likely to die. Patients who delay treatment beyond 24 hours have only a 20% survival rate. Coma at presentation means a 35% chance of death. A temperature above 105.8°F? That’s a 40% mortality risk.
Younger patients with Graves’ disease who skip their meds or have a sudden infection are the most common demographic. Women are affected more than men, especially during or after pregnancy. But anyone with uncontrolled hyperthyroidism is at risk.
Can It Be Prevented?
Yes. Prevention is simple but often ignored. If you have Graves’ disease or toxic nodules:
- Take your medication every single day. No exceptions.
- Never stop cold turkey, even if you feel fine.
- Get regular thyroid blood tests-every 3 to 6 months.
- Treat infections immediately. Don’t wait for them to get worse.
- Inform all doctors you have hyperthyroidism before any surgery or procedure.
- Know the warning signs: sudden fever, racing heart, confusion, vomiting.
The American Association of Clinical Endocrinologists launched a Thyroid Storm Awareness Program in 2020. Since then, delayed diagnoses have dropped by 18%. Education saves lives.
Final Reality Check
Thyroid storm is rare. But when it happens, it’s brutal. It doesn’t care if you’re young, healthy, or "on top of your health." It strikes when you’re vulnerable. The good news? If you recognize it early and get to an ICU fast, you have a very real chance of survival. The key is knowing the signs-and acting before it’s too late. If you’re caring for someone with hyperthyroidism, learn these symptoms. If you have it yourself, never underestimate the power of your pills. This isn’t a condition you can gamble with. One missed dose, one ignored fever, one delayed trip to the ER-and everything changes.





Reviews
Thyroid storm is essentially the body’s version of a nuclear meltdown-no safety protocols, no fail-safes, just pure unregulated metabolic chaos. It’s terrifying how a single missed pill can cascade into multi-organ failure. I’ve seen endocrinology residents freeze when the Burch-Wartofsky score hits 48. The real tragedy isn’t the storm itself-it’s how often it’s preventable. We treat hypertension like a lifestyle crime, but hyperthyroidism? People treat it like a suggestion. We need systemic education, not just patient handouts.
THEY’RE LYING TO YOU!! 😡 The pharmaceutical companies don’t want you to know that iodine therapy is 100% effective and they make 0 profit off it!! 🤫 They push methimazole because it’s a cash cow!! 🤑 My cousin took 200mg of potassium iodide daily for 3 weeks and her T3 dropped from 18 to 2.1 in 21 days!! 📉 The FDA is in bed with Big Pharma!! 🏥💀 #ThyroidTruth #StopTheLies
Oh, darling, how quaint-your ‘ICU protocol’ reads like a medical textbook written by someone who’s never held a stethoscope in a real human crisis. Let’s be honest: the real ‘storm’ is the medical-industrial complex’s insistence on treating symptoms while ignoring the soul’s imbalance. You speak of beta-blockers like they’re saints, but have you considered the energetic resonance of the thyroid? The body doesn’t ‘overproduce’-it’s screaming for alignment. Propylthiouracil? A chemical bandage on a spiritual wound. 🌿✨
PTU is outdated. Methimazole is first-line now. Also, the 8-25% mortality stat is outdated-2023 meta-analysis shows 12%. And no, you don’t need 600mg PTU unless you’re in cardiac arrest. Also, typo: ‘thyroid storm’ not ‘thyroid storm.’
While the clinical description is largely accurate, the tone is alarmist and lacks scholarly restraint. The assertion that ‘death is likely’ without ICU care is statistically misleading-survival is not binary, and outcomes are heavily modulated by comorbidities. Furthermore, the recommendation to administer 80mg methimazole as a loading dose exceeds current ATA guidelines, which cap initial dosing at 40mg. This article reads less like a medical bulletin and more like a fear-mongering op-ed.
USA is the only country that lets Big Pharma control thyroid meds. In Germany, they test you every 2 weeks and give free iodine. Here? You get a 30-day script and a pat on the head. 🇺🇸👎 My sister died because her doctor said ‘it’s probably anxiety.’ I’m not mad-I’m just disappointed. 🇺🇸💔 #HealthcareIsACrime
My abuela had this in the ‘80s in Manila. No ICU, no fancy labs-just a priest, some ginger tea, and a cold towel on her forehead. She lived to 92. Sometimes the body knows how to heal itself if you just stop fucking with it. 🌏❤️
Philip, your abuela’s story is beautiful-but it’s an anecdote, not a protocol. We don’t memorialize survivors of untreated sepsis and say, ‘See? Antibiotics are unnecessary.’ Medicine isn’t about nostalgia. It’s about evidence. That said-I get it. There’s a deep cultural yearning to trust the body’s wisdom. But when your T3 is 18 and your heart’s at 150, ‘ginger tea’ is the last thing on the ICU nurse’s checklist. The real tragedy isn’t modern medicine-it’s the systems that let people get this far without care.