Antacid-Antibiotic Timing Calculator
Calculate Safe Timing Between Antibiotics and Antacids
Ensure your antibiotics work effectively by spacing them correctly from antacids. This tool calculates the minimum time you should wait based on the antibiotic type and when you took the antacid.
Recommended Timing
Important: This tool provides general guidance based on clinical evidence. Always consult your doctor or pharmacist for personalized advice.
Many people reach for an OTC antacid like Tums, Maalox, or Mylanta when they feel heartburn or indigestion. It’s quick, easy, and works fast. But if you’re also taking an antibiotic - say, for a sinus infection, urinary tract infection, or pneumonia - you could be quietly sabotaging your treatment. The problem isn’t just a myth. It’s a well-documented, clinically significant interaction that can lead to treatment failure, longer illness, and even antibiotic resistance.
Why Antacids Interfere with Antibiotics
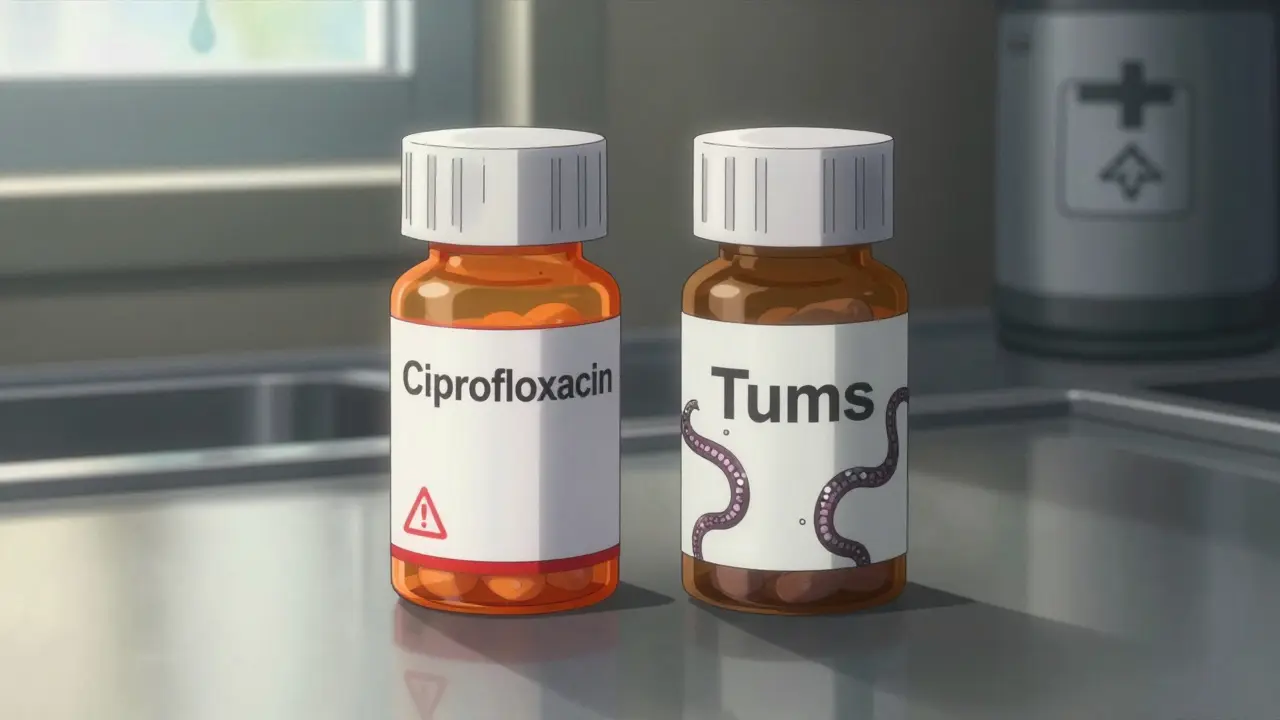
The issue comes down to chemistry. Many OTC antacids contain metal ions like aluminum, magnesium, or calcium. These metals don’t just neutralize stomach acid - they also bind tightly to certain antibiotics in your gut. This binding forms insoluble complexes that your body can’t absorb. The result? The antibiotic passes through you without ever reaching the infection site. This isn’t true for all antibiotics. The big ones affected are tetracyclines (like doxycycline) and fluoroquinolones (like ciprofloxacin and levofloxacin). Studies show that when taken with an antacid, tetracycline absorption can drop by 70-90%. Ciprofloxacin drops from 70% bioavailability to as low as 15-25%. That’s not a small drop - it’s the difference between a cure and a lingering infection. Even amoxicillin, which many assume is safe, isn’t completely immune. One study found its absorption dropped by 18-22% when taken with aluminum-magnesium antacids. Other antibiotics like diclofenac and metformin are also affected, but antibiotics are the most concerning because their job is to kill bacteria - and if they don’t reach the right concentration, they can’t do it.Which Antacids Are the Worst?
Not all antacids are created equal. The ones with aluminum hydroxide, magnesium hydroxide, or calcium carbonate are the biggest culprits. Here’s what’s in your typical bottle:- Aluminum hydroxide - Found in Maalox, Mylanta, and Gaviscon. Strong chelator.
- Magnesium hydroxide - Also in Maalox and Mylanta. Works fast, binds tightly.
- Calcium carbonate - The main ingredient in Tums. Often overlooked, but just as problematic.
- Sodium bicarbonate - Less common now, but still in some products. Can interfere differently.
How Much Does This Really Affect Treatment?
It’s not just theory. Real patients have had treatment fail because of this. One case from University Hospitals in March 2024 involved a woman with recurring UTIs. She took ciprofloxacin as prescribed - but also chewed two Tums tablets every time she felt bloated. Her urine cultures kept showing the same bacteria. Only after her doctor asked about her antacid use did the connection become clear. Once she stopped taking Tums within 4 hours of her antibiotic, her infection cleared in days. A 2023 meta-analysis found that people who took antacids at the same time as their antibiotics had a 37% higher chance of treatment failure. That’s not a small risk. That’s nearly 4 in 10 people getting sicker because of a simple timing mistake. And it’s not just about not getting better. When antibiotics don’t reach effective levels, bacteria survive. Those survivors multiply. Over time, that’s how antibiotic resistance starts. The CDC estimates over 35,000 deaths in the U.S. each year come from infections that no longer respond to standard antibiotics. This interaction contributes to that crisis.
When and How to Take Them Separately
The fix is simple: time it right. For tetracyclines (doxycycline, minocycline): Take the antibiotic at least 2 hours before or 4 hours after the antacid. For fluoroquinolones (ciprofloxacin, levofloxacin): Wait 4 to 6 hours after taking the antacid before taking the antibiotic. Some guidelines say 2 hours before - but 4+ is safer. For amoxicillin: While the effect is smaller, it’s still there. Best to separate by 2 hours if possible. Don’t just space them out randomly. Use a clock. Set a reminder on your phone. Write it down. This isn’t something you can eyeball. If you’re taking antacids for chronic heartburn, talk to your doctor about switching to an H2 blocker or PPI during your antibiotic course. These won’t interfere with absorption. They just take longer to work - so plan ahead.Why Most People Don’t Know This
You’d think this would be common knowledge. But a 2022 survey found only 32% of OTC antacid users knew about the risk of antibiotic interactions. Even though the FDA required warning labels on packaging in 2019, a 2022 audit showed only 67% of major brands fully complied. Pharmacists are on the front lines. They see patients buy Tums and ciprofloxacin together at the same counter. But many patients don’t ask. They assume “over-the-counter” means “safe with everything.” That’s a dangerous assumption. Reddit threads like r/pharmacy have dozens of posts from people who thought their antibiotic wasn’t working - until they realized they were taking antacids with it. One user wrote: “I took cipro for 5 days and felt worse. My pharmacist asked if I was taking Tums. I said yes. He told me to stop. Next day I felt better.”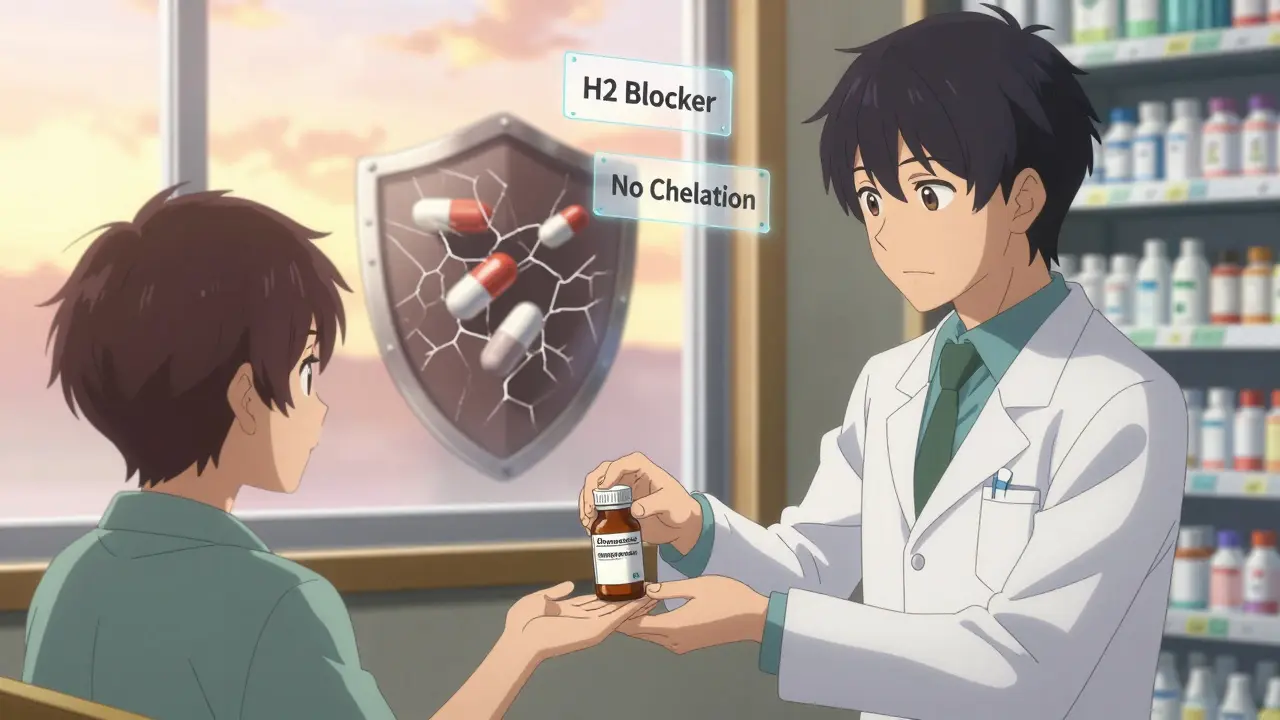
What You Should Do
If you’re prescribed an antibiotic:- Check the label. Does it say “avoid antacids”? If yes, take it seriously.
- Look at your antacid. Does it contain aluminum, magnesium, or calcium? If yes, separate doses by at least 2 hours - 4 is better.
- Don’t take antacids right after your antibiotic. Wait. Use a timer.
- If you have frequent heartburn, ask your doctor if you can switch to famotidine or omeprazole while on antibiotics.
- When in doubt, ask your pharmacist. They’re trained to catch these interactions.
Alternatives to Antacids During Antibiotic Treatment
You don’t have to suffer heartburn while on antibiotics. Here are safer options:- H2 blockers - Famotidine (Pepcid), ranitidine (if still available). Start 30-60 minutes before meals. No metal ions. No chelation.
- Proton pump inhibitors - Omeprazole, esomeprazole. Take 30-60 minutes before breakfast. Slower onset, but no direct interaction with antibiotics.
- Lifestyle tweaks - Avoid spicy foods, eat smaller meals, don’t lie down after eating. These help reduce acid without drugs.
Final Thought: Don’t Assume It’s Safe
Just because something is sold over the counter doesn’t mean it’s harmless. Antacids are powerful enough to change how your body absorbs life-saving drugs. That’s not a side effect - it’s a major drug interaction. If you’re on antibiotics, treat your antacid like a second medication. Time it. Track it. Talk about it. Your body will thank you.Can I take Tums with amoxicillin?
It’s not recommended. While amoxicillin is less affected than tetracyclines or fluoroquinolones, studies show its absorption can drop by 18-22% when taken with aluminum-magnesium antacids like Tums. To be safe, separate them by at least 2 hours. If you’re on amoxicillin and have heartburn, ask your doctor about switching to famotidine or omeprazole instead.
How long should I wait between antacids and antibiotics?
For tetracyclines like doxycycline, wait at least 2 hours before or 4 hours after taking the antacid. For fluoroquinolones like ciprofloxacin, wait 4 to 6 hours. If you’re unsure, wait 4 hours - it’s the safest window for most antibiotics. Don’t guess. Use a timer or phone alarm.
Do all antacids interfere with antibiotics?
No. Only antacids containing aluminum, magnesium, or calcium cause this interaction. Sodium bicarbonate can interfere too, but less commonly. Antacids with simethicone (like Mylanta) still contain aluminum or magnesium, so they’re risky. H2 blockers (famotidine) and PPIs (omeprazole) don’t contain these metals and are safer alternatives.
Can antacids make antibiotics completely useless?
They can come close. With ciprofloxacin and aluminum-containing antacids, absorption can drop from 70% to as low as 15%. That means the antibiotic isn’t reaching the infection in enough concentration to kill bacteria. This can lead to treatment failure, longer illness, and even the development of antibiotic-resistant strains.
What should I do if I accidentally took them together?
Don’t panic, but don’t ignore it. Take your next antibiotic dose at least 4 hours after the antacid. Don’t double up on the antibiotic. If you’re on a short course (5-7 days) and this happened once, you’re probably fine. But if it happens repeatedly, your treatment may fail. Tell your doctor or pharmacist - they may need to extend your course or switch antibiotics.




Reviews
People still take Tums with antibiotics? Honestly, this isn't even a debate. It's basic pharmacology. If you can't follow simple timing rules, don't blame the medicine.
Stop being lazy. Use a timer.
This is such an important post! 🙌 I literally just took cipro last week and had no idea about the Tums thing. I’ve already told my mom (who takes antacids daily) and my sister (who’s on doxycycline right now). Thank you for sharing this - it could literally save lives. 💪❤️
Okay, I’m officially shocked. I’ve been popping Tums with my amoxicillin for years because ‘it’s just a stomach thing.’
Turns out, I’ve been sabotaging my own recovery. No wonder I kept getting sick after antibiotics.
Now I’m switching to Pepcid - and I’m setting phone alarms for every dose. This is life-changing stuff.
Also, why isn’t this on every pharmacy flyer? Why isn’t it on the Tums box? I feel like I’m the only one who didn’t know this.
Thanks for making me smarter. I’m sharing this with my entire family.
And yes, I’m now the person who asks, ‘Did you take your antacid with your antibiotic?’ at every dinner.
Sorry not sorry.
Also, milk is not a substitute. I tried that once. Didn’t help. Just gave me gas.
TL;DR: Time your meds. Or suffer. Your call.
It’s not that hard to wait two hours. If you can scroll Instagram for 20 minutes, you can wait 120 seconds between pills.
Stop pretending you’re too busy to read the label.
This isn’t complicated. It’s careless.
Why do we even have OTC antacids if they’re this dangerous? Why isn’t the FDA just banning them? Or at least making them prescription-only? This isn’t a ‘timing issue’ - this is a systemic failure. People are dying because we treat medicine like candy. And now we’re blaming the patient? No. We’re blaming the system. The system that lets you buy calcium carbonate next to antibiotics like it’s a snack. This isn’t education. It’s negligence.
And don’t even get me started on how pharmacies still don’t screen for this. I’ve seen it myself - same counter, same transaction. No warning. No question. Just cash. Cash. Cash.
Someone needs to sue someone. I’m not joking.
It’s funny how we treat drugs like they’re either ‘safe’ or ‘dangerous.’ But everything is a spectrum. Water can kill you if you drink too much. Oxygen can poison you. Even sunlight gives you cancer. So why are we surprised that a substance that neutralizes stomach acid - which is literally hydrochloric acid - might interfere with another chemical designed to survive that same environment?
It’s not magic. It’s chemistry.
And yet, we act like the body is a magic box that just ‘knows’ what to do. It doesn’t. It’s a machine. And machines need instructions.
Maybe the real problem isn’t antacids.
It’s our belief that biology should be intuitive.
One must ask: Why is it that the most vulnerable populations - the elderly, the chronically ill, the economically disadvantaged - are precisely those who rely most heavily on OTC remedies? They are not given the luxury of time, education, or access to pharmacists who might intervene. This is not a personal failure - it is a public health catastrophe.
Let us not mistake ignorance for irresponsibility.
And let us not congratulate ourselves for knowing something that should have been common knowledge since the 1970s.
The failure lies not in the patient, but in the infrastructure that failed to educate them.
And until that changes, we are all complicit.
Hey, I just want to say - this is one of the most useful posts I’ve seen all year.
Thank you for laying it out so clearly.
I’m a nurse, and I’ve seen this exact thing happen too many times - patients come back with the same infection because they were taking Tums with their cipro. No one told them. No one asked.
So I’m sharing this with my team tomorrow. We’re making a handout. We’re putting it on our bulletin board. We’re printing it out and handing it to every patient who gets a fluoroquinolone or tetracycline.
And if you’re reading this and you’re on antibiotics - please, please, please - pause before you reach for that antacid.
Set a reminder. Write it on your hand. Do whatever it takes.
You’ve got this. And you’re not alone.
so like... tums = bad? with abx? wow. mind blown.
wait, so like... aluminum and mag? those are like... in like... rocks? and like... why does my stomach hurt if i dont take them? i mean... is it just... acid? or is it like... my soul crying?
anyway, i took cipro and tums together 3 times last week. i think i’m immune now? or dead? idk.
also, my dog ate a tums. is he gonna die? plz advise.
thx for the post tho. it was... kinda long. but cool.
According to the FDA’s 2019 guidance on drug interaction labeling, antacids containing polyvalent cations are required to include warnings regarding concomitant administration with tetracyclines and fluoroquinolones. The cited meta-analysis (2023) reported a 37% increase in treatment failure, with a 95% confidence interval of 31–43%. Absorption reductions for ciprofloxacin range from 55% to 85%, depending on formulation and timing. The clinical significance is unequivocal. Noncompliance remains the primary barrier to therapeutic efficacy in this context. The solution is behavioral, not pharmacological.
Why are you all acting like this is new? My mom has been on antibiotics since 2010 and she never takes antacids with them. You people are just lazy. And now you’re acting like you discovered fire.
Also, if you can’t read a label, maybe you shouldn’t be taking medicine at all.
Stop making this a big deal. Just do it right.
Hey everyone - I’m a pharmacy tech in Delhi, and I see this every single day.
People buy amoxicillin and Tums together, no questions asked. I try to warn them, but most just say, ‘Oh, it’s just a little heartburn, I’ll be fine.’
So I started writing little notes on the bag: ‘Wait 4 hours between Tums and antibiotic.’
Some people ignore it. But others? They come back and thank me.
One lady told me she’d been sick for 3 weeks - then stopped taking Tums with her doxycycline and felt better in 2 days.
It’s not about being perfect. It’s about being aware.
And if you’re reading this - you’re already ahead of most.
Keep going. You’re doing better than you think.