When you have COPD, breathing gets harder-not just because of your lungs, but because your muscles are wasting away. This isn’t just about getting older. It’s sarcopenia-a dangerous loss of muscle mass, strength, and movement that affects nearly 1 in 5 people with COPD. And if left unaddressed, it can cut your life short by decades. The good news? You can fight it. With the right nutrition and a smart resistance training plan, many people with COPD regain the ability to walk, climb stairs, and even carry groceries again.
What Is Sarcopenia in COPD, and Why Does It Matter?
Sarcopenia isn’t just weak muscles. It’s a medical condition where your body loses muscle faster than it can rebuild it. In COPD, this happens at twice the rate of normal aging. While healthy older adults lose about 1-2% of muscle mass each year, people with COPD lose 3-4%. That’s why so many patients say they feel like they’re “shrinking” from the inside.
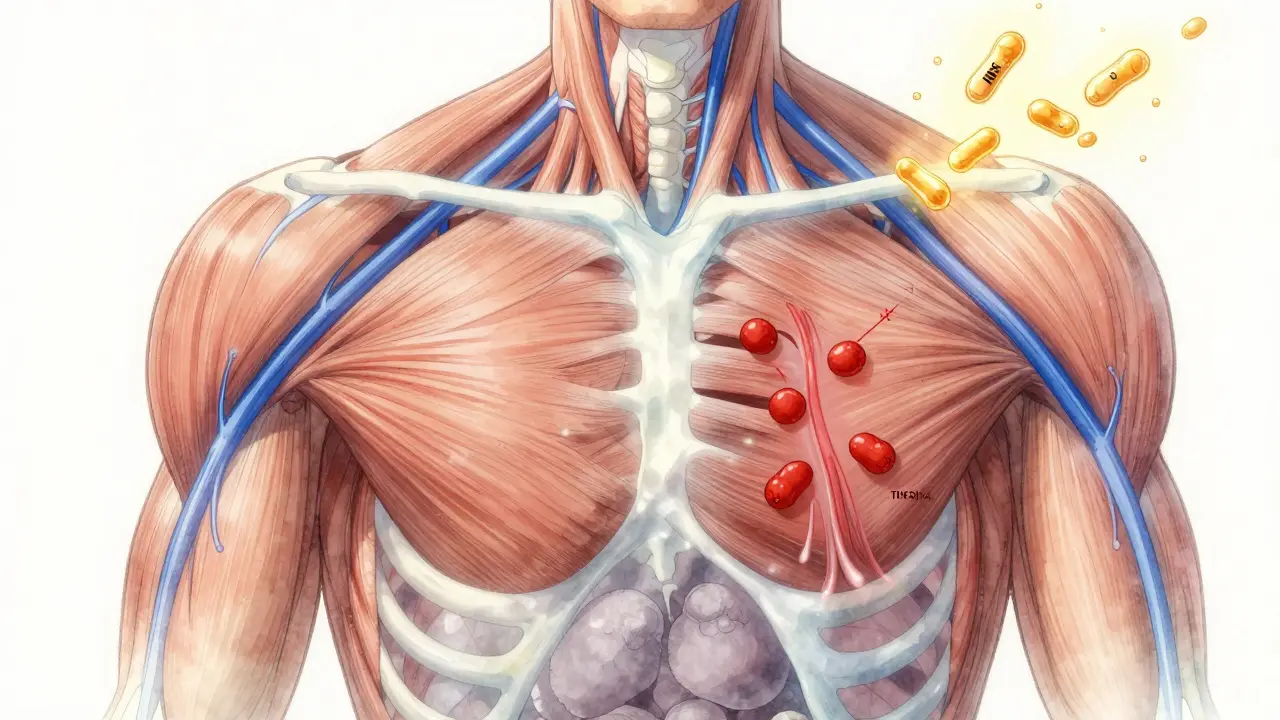
What makes this worse is that the muscle loss doesn’t just hit your legs. It hits your breathing muscles-the diaphragm, the intercostals, even your chest muscles. In fact, 68% of COPD patients show major atrophy in the pectoralis muscle, compared to only 22% of healthy people their age. That means even simple tasks like lifting a coffee cup or opening a jar become exhausting.
The consequences are severe. Studies show COPD patients with sarcopenia have a 20-40% higher risk of dying within five years. They’re also 32% more likely to end up in the hospital. This isn’t just about quality of life-it’s about survival.
How Is Sarcopenia Diagnosed in COPD?
Doctors don’t just guess. There are clear, measurable ways to spot sarcopenia early.
The first sign is muscle strength. A simple handgrip test using a dynamometer tells you a lot. If your grip is below 27 kg for men or 16 kg for women, that’s a red flag. But strength alone isn’t enough. You also need to check muscle mass. The best way? A DEXA scan or a CT scan at the L3 level of your spine. For men, a muscle index under 55 cm²/m², and for women, under 39 cm²/m², means you’re losing muscle faster than you should.
There’s also the Short Physical Performance Battery (SPPB), which measures how fast you walk 4 meters, how long you can stand on one foot, and how well you rise from a chair. A score of 8 or lower means your physical performance is in the danger zone.
And here’s something unique to COPD: your pectoralis muscle index (PMI). A value below 1.06 cm²/BMI is a strong predictor of sarcopenia in COPD patients-more accurate than BMI alone, which often misses the problem because people with COPD are often thin but still losing muscle.
Why Standard Sarcopenia Plans Don’t Work for COPD
Many people assume sarcopenia treatment is the same no matter the cause. But COPD is different. In heart failure or kidney disease, muscle loss comes from poor circulation or toxins. In COPD, it’s a perfect storm: low oxygen, constant inflammation, lack of movement, and not enough protein.
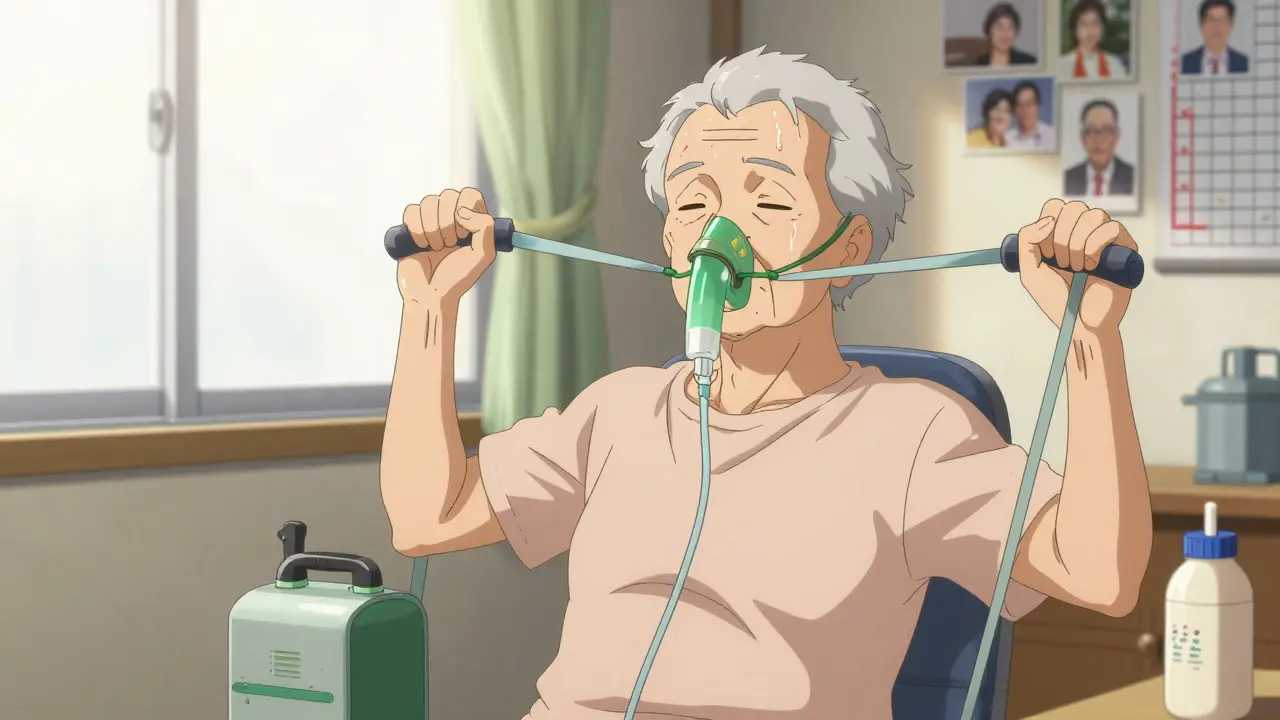
One big difference? Your breathing. When you lift weights, your body needs more oxygen. But if your lungs are already struggling, you can’t just do a standard gym routine. Forty-two percent of COPD patients need supplemental oxygen during resistance training. If you don’t plan for that, you’ll feel dizzy, breathless, and quit before you see results.
Also, inflammation is a silent driver. High levels of TNF-alpha and IL-6 in your blood directly attack muscle tissue. These markers are stronger predictors of muscle loss than age or smoking history. So treating sarcopenia in COPD isn’t just about lifting weights-it’s about reducing inflammation through diet, oxygen therapy, and pacing your activity.

Nutrition: The Missing Piece in COPD Care
Most COPD patients eat too little protein. On average, they get only 0.9 grams per kilogram of body weight. The recommended amount for sarcopenia? 1.2 to 1.5 grams per kilogram. That’s a 30-70% increase.
But it’s not just about quantity. Timing matters. Your muscles can only use so much protein at once. Spreading your intake across 4 meals-each with 0.3 to 0.4 grams per kilogram-is far more effective than loading up at dinner.
For example: If you weigh 70 kg, aim for 21 grams of protein per meal. That’s about 3 eggs, 100 grams of chicken, or one scoop of whey protein with 10 grams of leucine. Leucine is the key amino acid that turns on muscle growth. Studies show adding 2.5 to 3 grams of leucine per meal boosts muscle synthesis by 37% in COPD patients.
Many struggle with appetite. COPD makes eating tiring. Solutions? Use liquid supplements. A high-protein shake with leucine between meals can make a huge difference. Avoid sugary drinks-focus on protein and healthy fats. Some patients do better with smaller, more frequent meals. And if you’re on long-term steroids, your protein needs go even higher-up to 1.6 g/kg/day.
Resistance Training: How to Start Without Worsening Your Breathing
You don’t need a gym. You don’t need heavy weights. You need consistency.
Start at 30% of your one-rep maximum. That’s light-think 1-2 pound dumbbells or resistance bands. Do 2-3 sets of 10-15 reps for each major muscle group: chest, back, shoulders, legs. Focus on slow, controlled movements. Breathe out when you push or lift. Breathe in when you lower or relax.
Rest 2-3 minutes between sets. This isn’t a cardio workout. It’s muscle rebuilding. If you’re short of breath, stop. Don’t push through it. Use supplemental oxygen if you have it. Many patients don’t realize they can-and should-use it during exercise.
Progress slowly. After 4-6 weeks, if you’re not gasping, increase the resistance by 5-10%. It might take 8-12 weeks to feel stronger, but the gains are real. One study showed a 23% improvement in 6-minute walk distance after 16 weeks of supervised training. That’s the difference between needing help to get to the bathroom and walking to the kitchen alone.
Best exercises for COPD patients:
- Seated chest press with bands
- Wall push-ups
- Chair squats (hold onto a sturdy surface)
- Seated leg extensions with ankle weights
- Standing calf raises (hold onto a counter)
Do this 2-3 times a week. Even 20 minutes a session is enough to start. And always pair it with your pulmonary rehab program if you have one.
What Works in Real Life
Real patients aren’t lab subjects. Their stories tell the truth.
Mary Thompson, 68, with GOLD Stage 3 COPD, started with resistance bands and a protein shake after breakfast. After 12 weeks, she could carry her groceries without stopping. “I didn’t think I’d ever do that again,” she said.
John Peterson, 72, with Stage 4 COPD, tried resistance training without oxygen. He quit after three sessions. “I felt like I was drowning,” he said. “No one told me I could use my oxygen during exercise.”
The difference? Support. Patients who got guidance from a pulmonary rehab specialist had a 68% success rate. Those who tried on their own? Only 32% stuck with it.
And it’s not just about strength. People report better sleep, less anxiety, and more confidence. They stop canceling plans. They start going out again.
Barriers and How to Overcome Them
Here’s the hard truth: most clinics still don’t screen for sarcopenia. Only 38% of U.S. pulmonary rehab centers check handgrip strength or muscle mass. That means many patients slip through the cracks.
Common roadblocks:
- Dyspnea during exercise: Use oxygen. Start lighter. Take longer breaks.
- Lack of protein: Add a whey protein shake with leucine to breakfast and lunch.
- Exacerbations: Pause training during flare-ups, but resume as soon as you’re stable. Even light movement helps prevent further loss.
- No access to rehab: Ask your doctor for a referral. If none is available, use YouTube videos from certified pulmonary rehab programs. Look for ones labeled “COPD-safe resistance training.”
And don’t wait for perfection. If you can’t do a full workout, do 5 minutes. If you can’t get protein from food, use a supplement. Small steps still move the needle.
The Future: What’s Coming Next
Research is moving fast. In 2024, GOLD released the first-ever algorithm for managing sarcopenia in COPD. It links oxygen levels during sleep to exercise prescriptions. If your oxygen drops below 88% for more than 30% of the night, your training intensity should be lower.
New drugs are also in the pipeline. A myostatin inhibitor called PTI-501 is in phase 2 trials and could help block muscle breakdown. Beta-hydroxy-beta-methylbutyrate (HMB), a natural compound found in milk and meat, is being tested in a major European trial to see if it can preserve muscle better than protein alone.
But the biggest breakthrough isn’t a drug. It’s awareness. By 2027, experts predict sarcopenia screening will be standard in all COPD care. Because the math is clear: fixing muscle loss cuts hospital stays by a third and adds nearly half a year to your quality-adjusted life.
This isn’t about extending life. It’s about making every day worth living.
Can sarcopenia be reversed in COPD patients?
Yes, sarcopenia can be reversed-even in advanced COPD. Studies show that with consistent resistance training and adequate protein intake (1.2-1.5 g/kg/day), patients can gain muscle mass and strength within 8-16 weeks. The key is starting slow, using proper oxygen support, and sticking with it. Even small gains in grip strength or walking distance improve survival and independence.
How much protein should a COPD patient with sarcopenia eat daily?
A COPD patient with sarcopenia should aim for 1.2 to 1.5 grams of protein per kilogram of body weight per day. For example, a 70 kg person needs 84-105 grams of protein daily. This should be split evenly across 4 meals (about 21-26 grams per meal) to maximize muscle protein synthesis. Adding 2.5-3 grams of leucine per meal (found in whey protein or supplements) can boost results by up to 37%.
Is resistance training safe for someone with severe COPD?
Yes, when done correctly. Start with very light resistance-1-2 pound dumbbells or resistance bands-and perform exercises seated or while holding onto a stable surface. Use supplemental oxygen if prescribed. Rest 2-3 minutes between sets. Avoid holding your breath. Many patients with severe COPD improve significantly with this approach. The biggest risk is not exercising, which leads to faster decline.
Why do COPD patients lose muscle faster than others?
COPD patients face a triple threat: chronic inflammation (elevated TNF-alpha and IL-6), low oxygen levels (especially at night), and physical inactivity due to breathlessness. These factors trigger muscle breakdown and block muscle repair. Studies show muscle mass declines at 3.2% per year in COPD versus 1-2% in healthy aging. The pectoralis and respiratory muscles are especially vulnerable, making everyday tasks harder.
Should I use protein supplements for sarcopenia in COPD?
Yes, especially if you struggle to eat enough protein. Whole foods are ideal, but many COPD patients have poor appetite or get tired eating. A whey protein shake with 10 grams of leucine, taken after exercise or between meals, is a practical solution. Look for supplements with at least 25 grams of protein and 2.5-3 grams of leucine per serving. Avoid sugary formulas-choose ones with minimal additives.
How often should I do resistance training with COPD and sarcopenia?
Start with 2 sessions per week, allowing at least 48 hours between workouts. Each session should last 20-30 minutes and focus on major muscle groups: legs, chest, back, and shoulders. As you get stronger, you can increase to 3 times per week. Always listen to your body-if you’re short of breath, stop and rest. Consistency matters more than intensity.





Reviews
It's funny how we think of muscles as just strength, but they're also the quiet keepers of our breath. In India, we say 'sharir ki shakti, pran ki shakti' - body strength is life strength. This post reminds me of my uncle who stopped walking after he got COPD, until someone showed him how to lift water bottles while sitting. He didn't need a gym. He needed someone to say, 'You can still do this.'
It's not about being strong. It's about not giving up on yourself.
And protein? We eat dal and eggs. Simple. But enough. If we can do it with rice and lentils, why make it complicated?
The clinical data presented is robust and aligns with current GOLD guidelines. The emphasis on protein timing and leucine supplementation is particularly well-substantiated in recent meta-analyses. The integration of DEXA and PMI metrics into routine screening protocols represents a significant advancement in personalized pulmonary rehabilitation.
Further research into myostatin inhibitors and HMB supplementation is warranted, though cost-accessibility remains a barrier in underserved populations.
They don't want you to know this, but the real reason muscles waste is because Big Pharma doesn't profit from protein shakes and resistance bands. They make billions off oxygen tanks, inhalers, and hospital stays. They don't want you to heal on your own. Look at the stats - only 38% of clinics screen for sarcopenia? Coincidence? I think not.
And why is leucine so special? Because it's in milk. And milk is controlled by the dairy cartel. They want you buying their expensive supplements, not eating eggs and chicken like people used to.
Use your oxygen during exercise? That's not advice - that's a trap. They're conditioning you to depend on machines. Wake up.
Just eat real food. Move slow. Don't trust the system.
This made me cry a little 😭
I watched my grandma go from carrying groceries to needing help to sit up. She started doing chair squats with a towel and a protein shake after her tea. After three months, she laughed and said, 'I think I can wash my own hair now.'
It's not about being strong. It's about being able to do the small things that make life feel like yours again.
Thank you for writing this. I'm sharing it with my dad's doctor tomorrow 💙
This is one of the most comprehensive and clinically grounded summaries I've encountered on sarcopenia in COPD. The integration of objective metrics - grip strength, PMI, SPPB - with actionable nutritional and exercise protocols represents a paradigm shift in patient care.
I particularly appreciate the emphasis on oxygen utilization during resistance training. Too often, patients are discouraged from using supplemental oxygen during exertion due to outdated assumptions about dependency. This is not only medically unsound - it is detrimental.
Healthcare systems must prioritize screening and reimbursement for pulmonary rehab programs that include structured resistance training. The cost-benefit ratio is undeniable.
Let’s be honest - this is just another neoliberal biohacking narrative dressed up as medical wisdom. The real issue is systemic neglect. You think protein shakes fix sarcopenia? Please. The root cause is the collapse of the social fabric - the isolation, the poverty, the lack of community support. A 70-year-old in Lagos doesn’t have access to whey protein or DEXA scans. He has a bowl of yam and a chair. And yet, he walks ten kilometers to fetch water. His body adapts. His resilience is not a medical protocol - it’s a cultural inheritance.
Meanwhile, Western medicine commodifies survival. ‘Add leucine.’ ‘Use resistance bands.’ As if muscle mass is a product you can optimize like a Tesla battery. The real tragedy isn’t muscle loss - it’s the erasure of embodied dignity in favor of quantifiable metrics.
Next, they’ll sell you a COPD NFT that tracks your grip strength.
Stop treating the body like a machine. Start treating people like humans.
- Olukayode, Lagos, Nigeria (where we don’t need a CT scan to know when we’re losing ourselves.)
You people are missing the point. Everyone talks about protein and bands like it’s magic. But what about the real cause? Smoking. That’s it. If you didn’t smoke, you wouldn’t have COPD. If you didn’t have COPD, you wouldn’t have sarcopenia. So why are we wasting time on shakes and chair squats? Fix the root. Stop smoking. That’s the only real solution. Everything else is just patching a leaky boat while the ocean is rising. And don’t tell me about ‘past smokers’ - if you smoked for ten years, you still damaged your lungs forever. No amount of whey is going to undo that. You think your body forgets? It remembers. Every day. And now you want to fix it with a protein shake? That’s not science. That’s denial. You need to face the truth. Smoking killed your muscles. Not age. Not inflammation. You. And now you’re trying to buy your way out of it. Sad.
Finally, someone says it straight. This isn’t about fancy scans or protein shakes. This is about American healthcare being broken. My dad had COPD. He got a referral to rehab - took six months to get in. By then, he could barely stand. The system doesn’t care until you’re on the verge of dying. Then they throw a bunch of tests at you and charge you $2,000 for a DEXA scan.
Meanwhile, in other countries, people get basic care. No insurance maze. No waiting lists. Just a doctor who says, ‘Eat more protein. Lift something. Breathe with your oxygen.’
We don’t need more studies. We need access. We need it now.
And if you’re a doctor reading this - stop waiting for perfect protocols. Start helping. Now.