Antifungal Choice Advisor
Recommended Antifungal
Key Takeaways
- Diflucan (fluconazole) is an oral azole with excellent bioavailability and a broad Candida spectrum.
- Itraconazole offers better coverage of molds but requires acidic stomach for absorption.
- Voriconazole is the go‑to for invasive aspergillosis but carries higher visual side‑effects.
- Posaconazole provides the widest mold coverage, useful for prophylaxis in immunocompromised patients.
- Cost, drug interactions, and infection type dictate which alternative is most appropriate.
What is Diflucan (Fluconazole)?
Diflucan is a synthetic triazole antifungal marketed under the generic name fluconazole. It belongs to the azole class and works by inhibiting the fungal enzyme lanosterol 14α‑demethylase, which stops ergosterol synthesis and destabilises the cell membrane.Fluconazole is highly water‑soluble, absorbed >90% after oral dosing, and distributes well into CSF and eye fluids. The drug was approved by the FDA in 1990 and quickly became the standard for treating uncomplicated Candida infections.
How Diflucan Works and When It’s Used
Fluconazole’s mechanism of action makes it especially effective against yeast‑type fungi such as Candida albicans, C. glabrata, and C. tropicalis. Common indications include oral thrush, vaginal candidiasis, and systemic candidemia in non‑neutropenic patients. Because it penetrates the blood‑brain barrier, it’s also used for cryptococcal meningitis, often in combination with flucytosine.
Comparing Antifungal Alternatives
When clinicians consider a switch from Diflucan, they usually balance three factors: spectrum of activity, pharmacokinetics, and safety profile. Below is a quick glance at the most frequently discussed alternatives.
| Drug | Spectrum | Oral Bioavailability | Typical Use | Key Side Effects | Average Monthly Cost (USD) |
|---|---|---|---|---|---|
| Diflucan (Fluconazole) | Candida spp., Cryptococcus | ~95% | Vaginal thrush, systemic candidemia, cryptococcal meningitis | GI upset, elevated LFTs, QT prolongation (rare) | $25 |
| Itraconazole | Candida spp., Aspergillus, Histoplasma | ~55% (acidic stomach required) | Blastomycosis, histoplasmosis, chronic pulmonary aspergillosis | Hepatotoxicity, heart failure risk, GI irritation | $120 |
| Voriconazole | Broad mold coverage (Aspergillus, Scedosporium) | ~96% | Invasive aspergillosis, refractory candidiasis | Visual disturbances, photosensitivity, hepatotoxicity | $320 |
| Posaconazole | Very broad (Mucorales, Aspergillus, Candida) | ~80% (delayed‑release tablet) | Prophylaxis in neutropenic patients, mucormycosis | GI cramps, hypertension, liver enzyme rise | $450 |
| Ketoconazole (oral) | Limited Candida, dermatophytes | ~30% | Topical prep conversion, rare systemic use | Severe hepatotoxicity, adrenal suppression | $15 |
| Nystatin (oral suspension) | Predominantly Candida spp. | Negligible systemic absorption | Oral thrush, esophageal candidiasis (local) | Minimal systemic side effects | $10 |
When to Stick With Diflucan
If the infection is limited to yeast, the patient is not on medications that strongly inhibit CYP2C9/CYP3A4, and cost is a concern, Fluconazole remains the top choice. Its once‑daily dosing and low interaction burden make it ideal for outpatient therapy.
When an Alternative May Be Better
- Itraconazole shines for infections that involve mold organisms or deep‑seated histoplasmosis, but clinicians must ensure the patient’s stomach pH is adequate.
- Voriconazole becomes the drug of record for invasive aspergillosis, especially in neutropenic or transplant patients, despite its higher price and need for therapeutic drug monitoring.
- Posaconazole is the prophylactic workhorse for bone‑marrow transplant recipients because it covers rare molds like Mucorales.
- Ketoconazole is rarely used systemically today due to liver toxicity; it mostly appears in topical creams.
- Nystatin is perfect for localized oral thrush when systemic absorption isn’t needed.
Dosing, Drug Interactions, and Monitoring
Fluconazole’s standard adult dose for uncomplicated candidiasis is 100‑200mg daily, with loading doses of 400mg for severe infections. It is a moderate inhibitor of CYP2C9 and CYP3A4, so clinicians watch for interactions with warfarin, phenytoin, and certain statins. Routine liver function tests are advised for therapy beyond two weeks.
In contrast, itraconazole’s absorption is pH‑dependent; proton‑pump inhibitors can drop its bioavailability by >50%. Voriconazole requires trough level checks (1‑5µg/mL) to avoid neuro‑visual toxicity. Posaconazole’s delayed‑release tablet formulation improves predictability, yet clinicians still monitor for hypertension and hepatic enzymes.
Cost Considerations in 2025
The price gap is stark. A 30‑day generic fluconazole course averages $25, while voriconazole can exceed $300 for the same period. Insurance formularies often place fluconazole on the preferred tier, making it the default unless culture data dictate otherwise. For patients without coverage, generic fluconazole offers a cost‑effective solution with comparable efficacy for the majority of yeast infections.
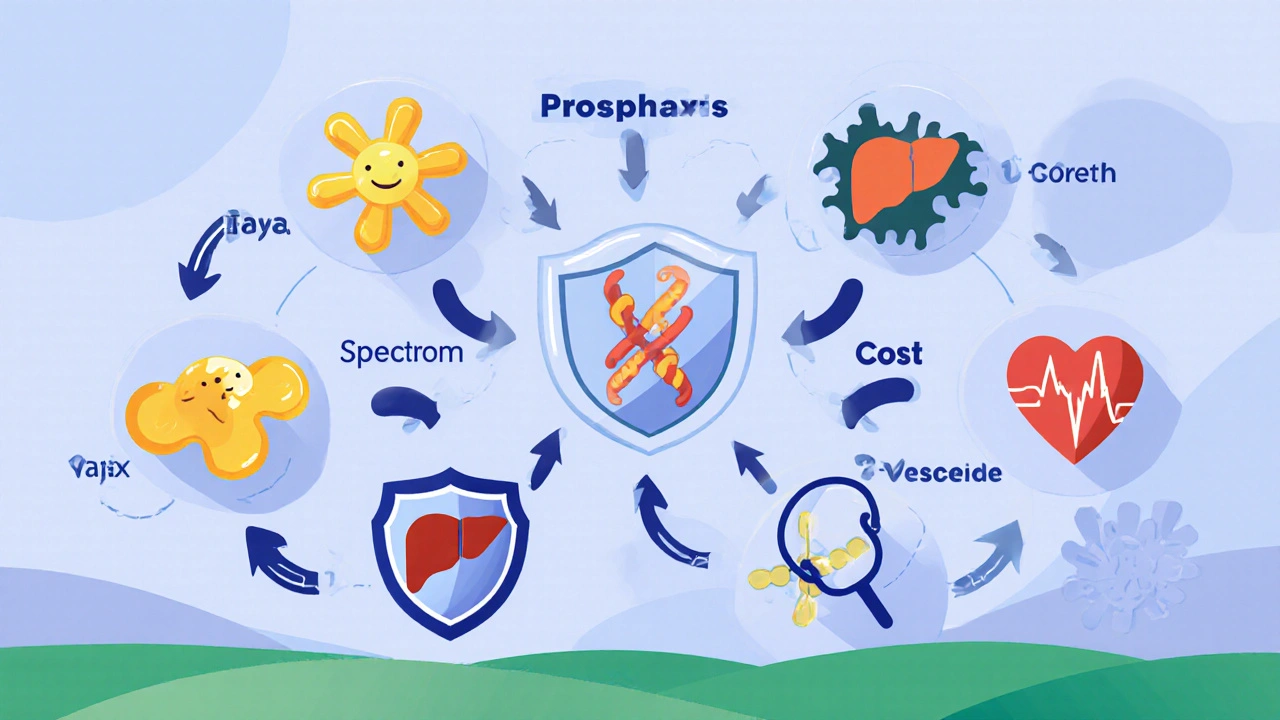
Decision Flowchart - Choosing the Right Antifungal
- Identify pathogen type: yeast vs. mold.
- If yeast and patient has no major CYP interactions → Diflucan.
- If mold or deep‑tissue infection → consider itraconazole (if Aspergillus, Histoplasma) or voriconazole (if invasive aspergillosis).
- For prophylaxis in immunocompromised hosts → posaconazole.
- Check hepatic function and concomitant meds before finalizing.
Practical Tips for Clinicians
- Obtain a culture whenever possible; species‑level data guide azole selection.
- Ask about over‑the‑counter antacids; they can sabotage itraconazole’s absorption.
- Educate patients on visual symptoms that warrant immediate discontinuation of voriconazole.
- For pregnant patients, avoid fluconazole high‑dose regimens due to teratogenic risk; consider topical nystatin instead.
- Leverage therapeutic drug monitoring for voriconazole and posaconazole in high‑risk cases.
Frequently Asked Questions
Can I use Diflucan for a skin fungus?
Fluconazole works best for yeast infections. Dermatophyte infections (e.g., athlete’s foot) respond better to terbinafine or topical allylamines. If a skin infection is proven to be Candida, a short course of fluconazole can be effective.
What should I watch for when taking voriconazole?
Patients often report blurred vision, colour changes, or photophobia within days of starting therapy. These symptoms are usually reversible after stopping the drug. Liver enzymes should be checked weekly for the first month.
Is fluconazole safe during pregnancy?
Low‑dose fluconazole (≤150mg weekly) is sometimes used for recurrent vaginal candidiasis, but high‑dose regimens have been linked to birth defects. Doctors typically prefer topical nystatin or clotrimazole for pregnant patients.
Why does itraconazole need an acidic environment?
Itraconazole’s capsule formulation dissolves best at low pH. Acid‑suppressing drugs raise stomach pH, reducing the drug’s solubility and leading to sub‑therapeutic blood levels.
When is posaconazole preferred over voriconazole?
Posaconazole is the drug of choice for prophylaxis against both Aspergillus and Mucorales in patients with prolonged neutropenia, such as those undergoing stem‑cell transplantation. Voriconazole covers Aspergillus well but lacks reliable activity against Mucorales.
Bottom Line
Diflucan remains the go‑to for uncomplicated yeast infections because it’s cheap, once‑daily, and has a predictable safety profile. When the pathogen is a mold, when drug interactions loom large, or when prophylaxis is needed, clinicians turn to itraconazole, voriconazole, or posaconazole based on the specific scenario. Understanding each agent’s strengths, weaknesses, and cost dynamics helps match the right antifungal to the right patient.





Reviews
Patriotism demands we protect our own health by choosing the cheapest effective drug. Fluconazole fits that bill, keeping costs low for American families.
The guide nicely outlines when fluconazole is appropriate and when alternatives are warranted. Its cost advantage is clear, especially for patients without complex comorbidities.
Exactly, keeping treatment affordable is key. For many yeast infections a single daily dose of fluconazole clears the infection quickly. If you need help dosing just ask.
Meh, another boring table.
Look, if you’re on a budget and not taking warfarin, fluconazole is the golden choice 😊. It avoids the hassle of acid‑suppressor issues that plague itraconazole.
Totally agree 😊. For patients worried about drug interactions, checking liver enzymes periodically while on fluconazole keeps things safe.
One must appreciate the lexical elegance of the term “fluconazole” juxtaposed against the prosaic “ketoconazole”. The former epitomizes pharmacological parsimony whilst the latter languishes in antiquated toxicity. In an era where cost‑effectiveness is tantamount to ethical stewardship, the judicious selection of fluconazole reflects a sagacious clinical philosophy.
i think the whole vibe is about balance not just price. fluconazole gives ya good coverage for most candida species. if you got mold you gotta go big or go home. the drug's bioavailability is stellar, so you can dose once daily. but dont forget the pH thing for itraconazole, that shit needs acid. taking antacids while on itraconazole is like pouring water on a fire. voriconazole, on the other hand, slaps hard on aspergillus but brings visual side effects. patients often report seeing halos or color shifts, which can freak them out. posaconazole is the probiotic of the lot, covering mucorales and more. however its price tag makes it a luxury item for most insurance plans. when you consider liver toxicity, fluconazole sits nicely in the low‑risk zone. regular LFT checks are still wise for any azole longer than two weeks. some clinicians still swear by therapeutic drug monitoring for voriconazole, and that's fine. the key takeaway is to match the drug to the pathogen and the patient's budget. so, in most outpatient yeast cases, stick with fluconazole and save the heavy hitters for the deep‑seated infections.
Listen up folks! If you’re still debating, just run the numbers – fluconazole saves you hundreds. No excuse for overprescribing pricey mold agents when a simple yeast infection is the culprit.
Calm down, Naresh. Many patients truly need the broader spectrum, and the physician’s judgment matters. Still, your reminder on cost is spot‑on.
I’ve seen several cases where a cheap generic fluconazole regimen cleared a stubborn candidemia in a non‑neutropenic patient. The key is to monitor liver enzymes if treatment extends beyond two weeks. Also, educating patients about possible QT prolongation, even if rare, builds trust.
Honestly, prescribing expensive drugs when fluconazole works is a moral failing. Doctors should prioritize what’s right for the patient, not the pharmaceutical lobby.
Let’s keep it professional. While cost is important, each case has its nuances and sometimes a higher‑priced agent is clinically justified. Respectful dialogue helps everyone.