More than 10% of people in U.S. hospitals carry a label saying they’re allergic to penicillin. But here’s the truth: over 95% of them aren’t actually allergic. That label? It’s often wrong. And it’s costing lives, money, and effective treatment options.
Maybe you got the label as a kid after a rash from amoxicillin. Or your mom said you were allergic because you got sick after taking it once. Maybe your doctor just checked a box on a form years ago and never questioned it again. But that label sticks - and it follows you into every hospital visit, every emergency, every infection. And it locks you out of the best, safest, cheapest antibiotics available.
Why a False Label Matters More Than You Think
When you’re labeled penicillin-allergic, doctors can’t use penicillin, amoxicillin, or other beta-lactam antibiotics - even if they’re the most effective choice. Instead, they turn to broader-spectrum drugs like vancomycin, clindamycin, or fluoroquinolones. These drugs are more expensive. They’re harder on your gut. And they fuel antibiotic resistance.
Here’s what that looks like in real numbers: patients with false penicillin allergy labels are 28% more likely to get fluoroquinolones and 69% more likely to get clindamycin than patients without the label. That’s not a coincidence. That’s a direct result of the label. And it’s driving up rates of drug-resistant infections like MRSA and ESBL-producing E. coli. The CDC estimates that false allergy labels contribute to 50,000 extra cases of C. diff infections every year in the U.S. alone - a dangerous, hard-to-treat gut infection that often leads to hospitalization.
And it’s expensive. On average, each false allergy label adds about $1,000 in extra healthcare costs per patient per year. Multiply that by millions of people, and you’re talking about billions wasted annually - money that could be spent on real care, not avoidable complications.
How Do You Know If Your Allergy Label Is Real?
Most people don’t know the difference between a true allergy and a side effect. A true IgE-mediated penicillin allergy causes symptoms like hives, swelling, trouble breathing, or anaphylaxis - usually within minutes to an hour of taking the drug. That’s rare. Less than 1-2% of people who say they’re allergic actually have this kind of reaction.
But most people who report a penicillin allergy had something else: nausea, diarrhea, a mild rash that wasn’t itchy, or a headache. Those aren’t allergies. They’re side effects. And they don’t mean you’re allergic for life.
Here’s the kicker: even if you had a real reaction decades ago, your body often outgrows it. Studies show that 80% of people who had a true penicillin allergy in childhood lose their sensitivity after 10 years. So if you were labeled allergic as a kid, there’s a very good chance you’re not allergic anymore.
The Testing Process: Simple, Safe, and Life-Changing
Getting tested isn’t complicated. And it’s safer than you might think. There are three main steps:
- History Review - Your provider will ask detailed questions about your reaction: What was the symptom? When did it happen? How long ago? Was it life-threatening? Tools like PEN-FAST help doctors quickly assess your risk. A score under 3 means you’re low risk - and you might not even need skin testing.
- Skin Testing - If you’re moderate risk, a specialist will do a skin prick test with tiny amounts of penicillin. No needles. Just a gentle poke. If that’s negative, they might do an intradermal test - still very low risk. These tests are 98% accurate at ruling out IgE-mediated allergies.
- Oral Challenge - If skin tests are negative, you’ll take a small dose of amoxicillin or penicillin under observation. You’ll be watched for 30-60 minutes. If nothing happens, you’re cleared. Then you’ll take a full therapeutic dose. That’s it.
Adverse reactions during testing? Less than 2% of cases - and most are mild, like a little rash or stomach upset. Severe reactions are extremely rare. In fact, the risk of a bad reaction during testing is lower than the risk of getting a dangerous infection because you couldn’t take the right antibiotic.
Some clinics skip skin testing and go straight to the oral challenge - especially for low-risk patients. Studies show 94.5% of these patients tolerate the drug without issue. It’s faster. It’s cheaper. And it works.
Who Can Do This Testing? You Don’t Need an Allergist
You might think you need to see an allergy specialist. But that’s not true anymore. Primary care doctors, pharmacists, and even nurses in many hospitals are now trained to do de-labeling. The American Academy of Allergy, Asthma & Immunology says non-allergists can safely do it - especially for low-risk patients - after just 10 supervised cases.
At the University of Pennsylvania Health System, they’ve de-labeled over 1,800 patients since 2020. Zero severe reactions. At Mayo Clinic, patients report being able to finally take amoxicillin for sinus infections instead of Z-Pak - which always gave them stomach problems. One 68-year-old woman in Massachusetts avoided three hospital stays for UTIs after her label was removed. She saved over $28,000 in two years.
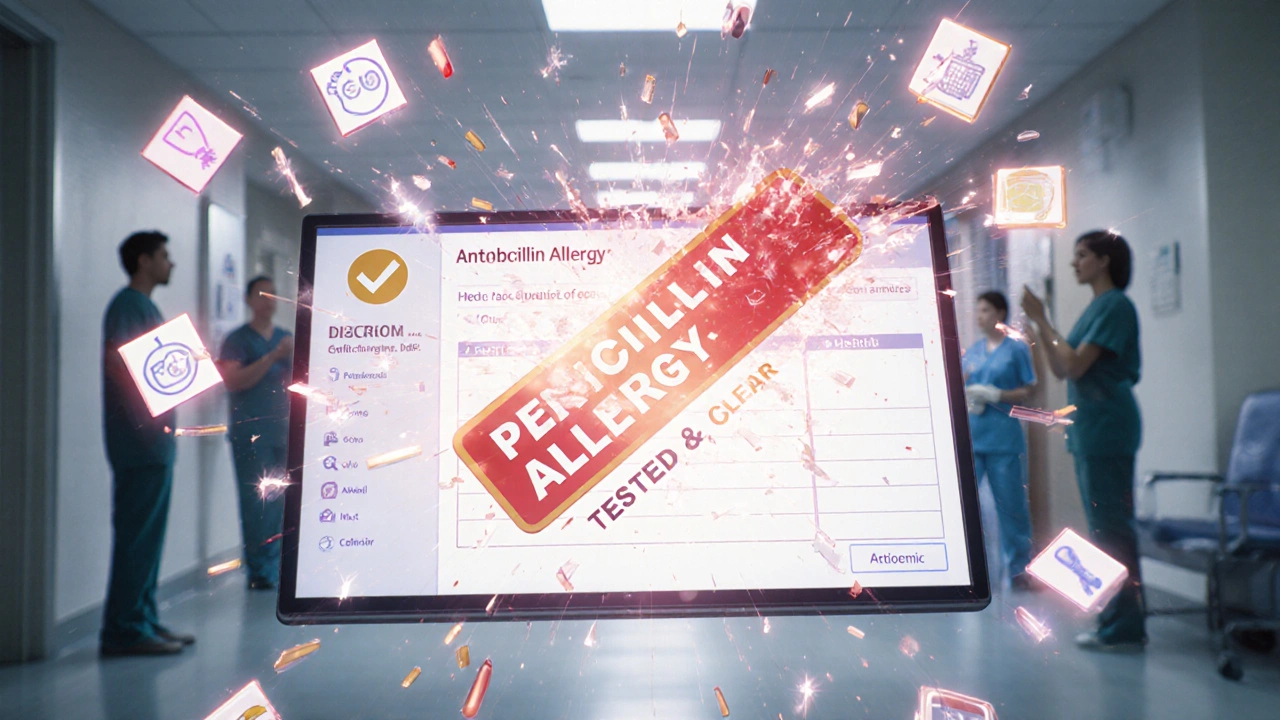
And it’s getting easier. Epic Systems, the EHR platform used by 84% of U.S. hospitals, now has a built-in tool that flags patients with penicillin allergy labels and suggests testing. Since 2021, it’s helped remove 198,000 false labels.
What Happens After You’re De-Labelled?
Once you’re cleared, your allergy record is updated - not just to say “penicillin allergy removed,” but to say “no penicillin allergy confirmed by testing.” That matters. Because if you’re labeled as allergic to “penicillin,” doctors might still avoid all related drugs, like amoxicillin or cefdinir. But cross-reactivity isn’t guaranteed. Your record should reflect which specific drugs you’re safe for.
And you’ll get a card or a note - sometimes digital - to carry with you. Next time you’re in the ER, you won’t have to argue. You’ll just say: “I was tested. I’m not allergic.”
Barriers Still Exist - But They’re Falling
Even with all the evidence, fewer than 40% of eligible patients get tested. Why? Long wait times. Lack of access. Fear. Misinformation.
Some people wait 14 weeks just to get an appointment. Others are told, “It’s too risky,” or “We don’t do that here.” But that’s changing. The CDC launched a $15 million initiative in 2024 to set up 12 regional de-labeling centers in underserved areas. The European Academy of Allergy and Clinical Immunology now supports telemedicine-based testing - and in the Netherlands, 96% of patients who did remote testing were successfully de-labeled with zero severe reactions.
And starting in 2025, Medicare will start measuring hospitals on how many false penicillin allergy labels they remove. That’s a game-changer. Hospitals will now be financially incentivized to fix this problem.
Your Next Step: Ask for a Test
If you’ve been told you’re allergic to penicillin - even once, even decades ago - you should ask your doctor about getting tested. Bring this up at your next appointment. Say: “I’ve been told I’m allergic to penicillin, but I’ve never had a serious reaction. Can we check if that’s still true?”
You don’t need a referral. You don’t need to be sick. You don’t need to wait. If you’ve avoided penicillin-based antibiotics for any reason, you’re a candidate for testing. And if you’re cleared, you’ll gain access to better, cheaper, safer treatments for every infection from now on.
This isn’t about changing your medical history. It’s about correcting a mistake - one that’s been costing you and the system far too much for far too long. Getting tested isn’t risky. Not getting tested is.
Can I outgrow a penicillin allergy?
Yes. Studies show that 80% of people who had a true penicillin allergy in childhood lose their sensitivity after 10 years. Even if you had a real reaction as a kid, it doesn’t mean you’re allergic for life. Testing can confirm whether your body still reacts.
Is skin testing painful or dangerous?
Skin testing is not painful. It’s done with a tiny prick, like a pinprick, and uses very small amounts of the drug. The risk of a reaction is less than 1%. Serious reactions are extremely rare. Most people feel nothing at all. The real danger is not testing - because it keeps you from using the best antibiotics when you need them.
What if I have a reaction during testing?
If you have a reaction during testing, it’s handled immediately. Testing is always done in a controlled setting with emergency equipment and trained staff on hand. Most reactions are mild - a small rash or itching - and easily treated. Even if you react, you’ll get a clear, accurate label. That’s better than living with a false one.
Can my pharmacist help me get tested?
Yes. In many hospitals and clinics, pharmacists are trained to screen patients for penicillin allergy and refer them for testing. Some community pharmacies even offer basic allergy risk assessments. Ask your pharmacist - they’re often the first to notice when a patient is being prescribed a less effective drug because of an outdated allergy label.
Will my insurance cover this testing?
Yes. Most insurance plans, including Medicare and Medicaid, cover drug allergy testing when it’s medically necessary. The cost of testing is typically under $200 - far less than the $1,000+ in extra costs caused by using broader-spectrum antibiotics. Many hospitals now include testing as part of routine care.
What if I’m allergic to something else - like sulfa or cephalosporins?
Penicillin allergy testing only confirms whether you’re allergic to penicillin and related beta-lactams. If you have a separate allergy to sulfa or cephalosporins, that’s a different issue. But many people confuse these. If you’re unsure, ask your provider for a full review. You might be avoiding more drugs than you need to.
Final Thought: This Isn’t Just About Penicillin
It’s about getting the right treatment when you’re sick. It’s about not being locked out of the best medicine because of an old mistake. It’s about reducing antibiotic resistance - a global crisis. And it’s about saving money, time, and unnecessary hospital stays.
If you’ve ever been told you’re allergic to penicillin, don’t assume it’s true. Ask for a test. You might be surprised what you find out - and how much better your care can be.






Reviews
So wait-you’re telling me I’ve been avoiding penicillin since I was 8 because I got a rash after amoxicillin? And now you want me to just swallow a pill in front of a nurse like it’s a candy? I’m not gonna risk anaphylaxis because some study says I’m ‘probably fine.’ My mom cried when I turned blue after that one dose-nope, not doing it.
It’s not merely a medical misclassification-it’s a semiotic failure of the biomedical apparatus. The penicillin-allergy label functions as a Foucauldian dispositif, disciplining patient autonomy through the epistemic violence of institutionalized diagnostic inertia. The very lexicon of ‘false allergy’ reifies a binary that pathologizes physiological variance. We must deconstruct the hegemony of the EHR’s algorithmic dogma and restore phenomenological agency to the embodied patient. 🌱
I work in a hospital pharmacy and see this all the time. So many patients are on clindamycin or levofloxacin for simple UTIs when amoxicillin would’ve cleared it in 2 days. One lady came in with a recurrent infection-turned out she’d been labeled allergic at age 5 after a stomach ache. We did the challenge, she’s fine now. No more GI nightmares. Just ask your doctor. It’s quick, safe, and free with insurance. Seriously, do it.
Oh wow, another feel-good article from Big Pharma’s PR team. ‘Just get tested!’ Like we all have time to wait 14 weeks for an appointment while our insurance denies coverage. And who’s gonna pay for the 3-hour clinic visit? Meanwhile, my doctor still won’t touch penicillin unless I sign a waiver. This is all just virtue signaling. Do better.
While I appreciate the intent of this piece, I’m concerned about the oversimplification of risk. Not every rash is ‘just a side effect.’ Some patients have delayed reactions that mimic allergies but aren’t IgE-mediated-those are still clinically significant. And while testing is great, we can’t assume all providers are adequately trained. Without standardized protocols, we risk creating new errors. Let’s improve access, yes-but also accountability.
I’ve been pushing this for years. My cousin got de-labeled last year after 22 years of avoiding all antibiotics. She’s now on amoxicillin for every infection. No drama. No extra cost. And guess what? Her doctor didn’t even charge her. This isn’t rocket science. It’s common sense. Why are we still treating this like it’s 1998? Stop being scared. Get tested. It’s not a threat-it’s a upgrade.
I’m 32 and was told I was allergic as a kid. Never had a bad reaction, just a little tummy upset. I never thought twice about it… until now. I’ll bring this up at my next checkup. Thanks for the nudge.
So let me get this straight… I’ve been paying extra for antibiotics I don’t need because my 5-year-old self got a rash after a cold? And now I’m supposed to be grateful someone finally figured out we’re all just… allergic to paperwork? 😑
OMG I just read this and my heart dropped. I’ve been avoiding penicillin since I was 6-got a rash, mom panicked, doctor checked the box. Now I’m 41 and get pneumonia every winter and they give me azithromycin which wrecks my stomach. I’m calling my doctor tomorrow. I’m not waiting anymore. I’ve had enough. This is insane. And I’m so glad someone finally said it out loud. Thank you. 💙