Hypothyroidism & Statin Myopathy Risk Calculator
Risk Assessment Tool
Enter your TSH level and statin type to see your risk of muscle damage.
When you’re on statins to lower cholesterol, the last thing you want is to start feeling muscle pain, weakness, or cramps. But if you also have untreated hypothyroidism, that risk jumps dramatically. It’s not just a coincidence - it’s a well-documented, dangerous interaction that many doctors still miss. And for millions of people managing both conditions, the consequences can be life-threatening.
Why Hypothyroidism Makes Statins More Dangerous
Statins work by blocking an enzyme your liver uses to make cholesterol. But they also interfere with something else: your muscles’ ability to produce energy. That’s where hypothyroidism comes in. When your thyroid isn’t making enough hormone, your muscles don’t get the energy they need to function properly. The result? A one-two punch that leaves your muscles vulnerable. Research shows that hypothyroidism slows down how your liver breaks down statins. The main enzyme involved, CYP3A4, becomes less active. That means more of the drug stays in your bloodstream - up to 50% higher levels in some cases. If you’re taking simvastatin or atorvastatin, that’s especially risky. These statins are processed by CYP3A4, and when your thyroid is underactive, your body can’t clear them fast enough. At the same time, statins reduce levels of coenzyme Q10 by 25-50%. This compound is essential for energy production in muscle cells. Hypothyroidism already lowers mitochondrial efficiency. Add a statin on top, and your muscles are running on empty. This is why muscle pain isn’t just a side effect - it’s a sign your cells are starving.The Numbers Don’t Lie
A 2019 study of over 12,000 patients found that people with TSH levels above 10 mIU/L had more than four times the risk of statin-induced myopathy compared to those with normal thyroid function. Even subclinical hypothyroidism - where TSH is between 4.5 and 10 - raised the risk by more than double. The real danger comes when TSH climbs higher. One case report described a woman whose TSH hit 22.4 mIU/L while she was still taking simvastatin 40 mg daily. Her creatine kinase (CK) levels soared to 28,500 U/L - over 500 times the upper limit of normal. She developed acute kidney failure and needed hemodialysis. That’s not rare. It’s preventable. On patient forums like PatientsLikeMe, 42.3% of hypothyroid users reported muscle symptoms on statins. Compare that to just 15.7% of people with normal thyroid function. And in a Healthline survey, 73% of hypothyroid patients who had muscle pain had TSH levels above 4.5 when symptoms started.Not All Statins Are Created Equal
If you have hypothyroidism, the type of statin you take matters as much as the dose. Lipophilic statins - like simvastatin, lovastatin, and atorvastatin - penetrate muscle tissue more easily. That makes them more likely to cause damage in people with thyroid issues. A 2021 meta-analysis showed that hypothyroid patients on simvastatin had a 12.7% chance of developing myopathy. That’s more than six times higher than the 2.1% risk in euthyroid patients. At doses of 40 mg or higher, simvastatin carries a 15.3-fold increased risk of rhabdomyolysis in this group. On the other hand, hydrophilic statins like pravastatin and rosuvastatin don’t enter muscle cells as easily. Pravastatin shows only a 1.3% myopathy rate in hypothyroid patients. Rosuvastatin at 10-20 mg/day has just a 1.4-fold increased risk compared to 3.2-fold for atorvastatin. That’s why the 2023 Endocrine Society guidelines recommend rosuvastatin as the first-choice statin for people with hypothyroidism.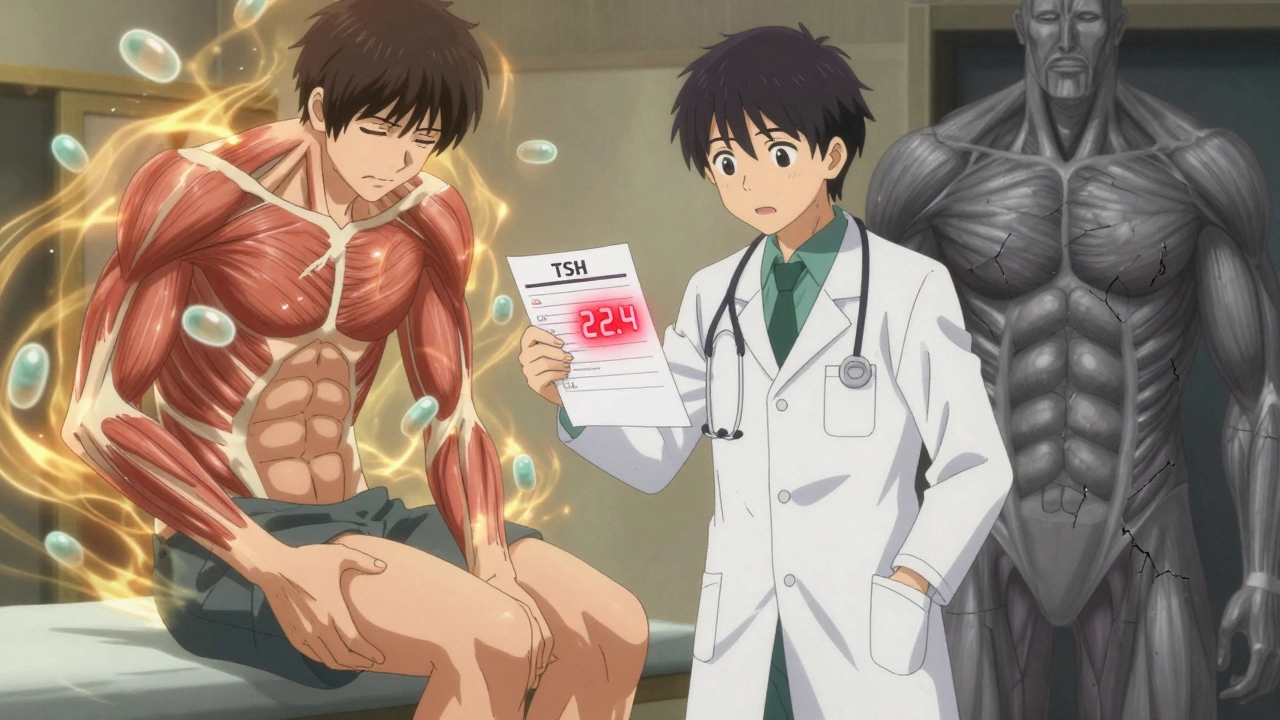
What Doctors Should Do - And Often Don’t
The American Thyroid Association and American College of Cardiology both recommend testing TSH before starting any statin. If you’re already on thyroid medication, your TSH should be checked every 6-8 weeks after starting or changing statin dose. The target? TSH between 0.5 and 3.0 mIU/L. But here’s the problem: many doctors don’t do this. A 2022 study found that over one-third of hypothyroid patients stopped their statins within a year because of muscle pain. Why? Because their thyroid wasn’t optimized first. In 89% of cases, those symptoms disappeared after adjusting levothyroxine - not by stopping the statin. Dr. Paul W. Ladenson from Johns Hopkins says treating hypothyroidism before starting statins reduces myopathy risk by 78%. That’s not a small gain. That’s the difference between keeping your medication and losing it.What You Can Do Right Now
If you’re on both levothyroxine and a statin:- Ask your doctor for your last TSH result. If it’s above 4.0, ask for a repeat test.
- If you’ve had muscle pain since starting a statin, get your TSH checked - even if you think you’re "fine" on thyroid meds.
- Don’t assume your statin is the problem. Your thyroid might be the missing piece.
- If your TSH is high, ask about adjusting your levothyroxine before considering stopping the statin.
- If you’re on simvastatin 40 mg or higher, ask if switching to rosuvastatin or pravastatin is an option.
Coenzyme Q10: Helpful, But Not a Fix
Some people take CoQ10 supplements hoping to ease muscle pain. A 2020 trial showed a 53.6% reduction in myalgia among hypothyroid statin users taking 200 mg daily. That sounds promising. But here’s the catch: CoQ10 doesn’t fix the root problem. It doesn’t lower your statin levels or improve your thyroid function. It’s like putting a bandage on a broken bone. It’s okay to try CoQ10 if your doctor agrees, but don’t rely on it. The real solution is fixing your thyroid.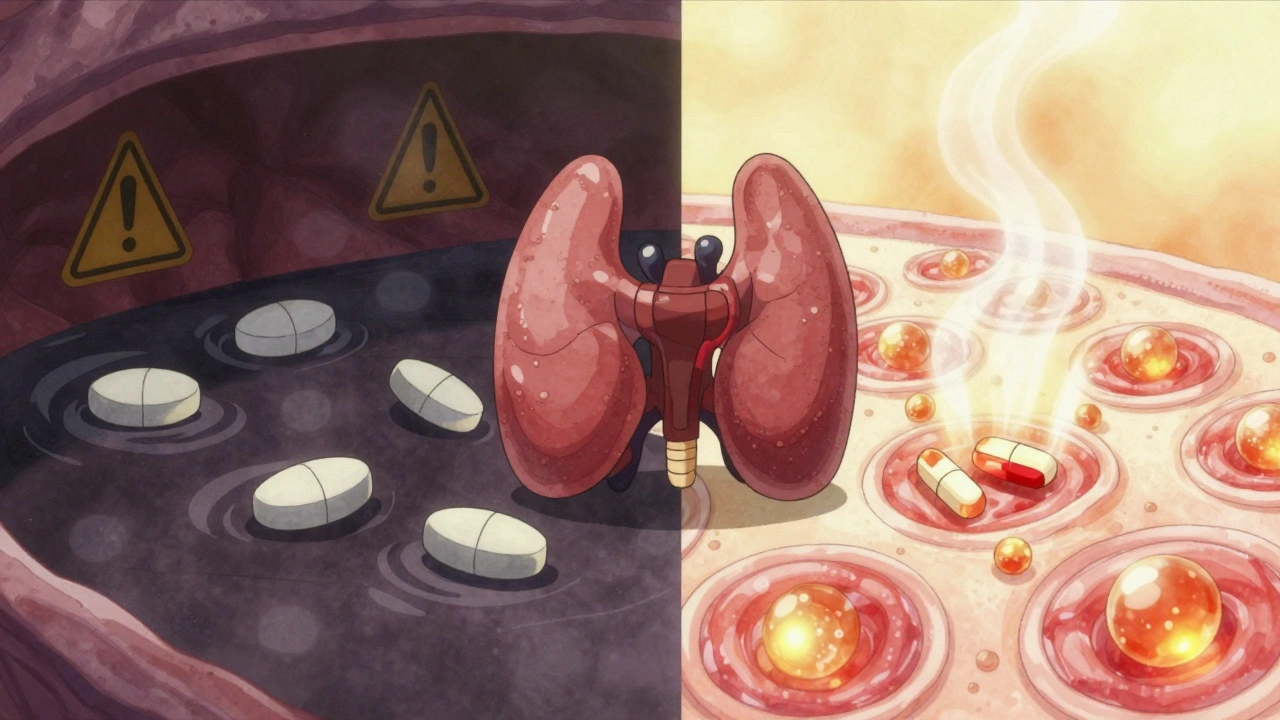
The Bigger Picture
About 20 million Americans have hypothyroidism. Nearly 40 million take statins. That means millions are walking around with this hidden risk. And because muscle pain is common with statins, many assume it’s just a side effect - not a warning sign. But here’s the truth: when thyroid function is optimized, 85-90% of hypothyroid patients can safely stay on statins. That’s not just about avoiding muscle pain. It’s about preventing heart attacks, strokes, and early death. A 2023 meta-analysis in Circulation showed that once thyroid levels are normal, hypothyroid patients on statins have the same cardiovascular outcomes as people with normal thyroid function. That’s huge. It means you don’t have to choose between protecting your heart and avoiding muscle pain. You just need the right management.What’s Changing in 2025
The FDA is drafting new guidance requiring thyroid testing before high-intensity statin therapy. The European Medicines Agency will soon require warning labels on all statin packages about this interaction. And researchers are developing a genetic risk calculator that combines thyroid function with SLCO1B1 gene variants to predict who’s most at risk. The THYROSIMVASTATIN trial, expected to release results in mid-2025, could change how we pick statins for people with thyroid disease - from guesswork to precision.Final Takeaway
Hypothyroidism doesn’t mean you can’t take statins. It means you need to take them smarter. Your thyroid isn’t just about energy or weight - it’s a key player in how your body handles medication. Ignoring it puts your muscles - and your heart - at risk. If you’re on both medications, get your TSH checked. If it’s above 4.0, talk to your doctor about adjusting your thyroid dose before doing anything else. Don’t quit your statin. Fix your thyroid. Then see if the pain goes away. For most people, it does.Can hypothyroidism cause muscle pain even without statins?
Yes. Hypothyroidism itself can cause muscle stiffness, cramps, and weakness because low thyroid hormone reduces energy production in muscle cells. Many people mistake this for general fatigue or aging. But when statins are added, the damage multiplies - making symptoms worse and more dangerous.
Should everyone with hypothyroidism avoid statins?
No. In fact, most people with hypothyroidism benefit from statins - if their thyroid levels are properly managed. The goal isn’t to avoid statins, but to optimize thyroid function first. Once TSH is in the target range (0.5-3.0 mIU/L), statins are generally safe and effective.
What’s the safest statin for someone with hypothyroidism?
Rosuvastatin and pravastatin are the safest options. They’re hydrophilic, meaning they don’t penetrate muscle tissue as easily as lipophilic statins like simvastatin or atorvastatin. Rosuvastatin at 10-20 mg/day has the lowest risk profile in hypothyroid patients, according to current guidelines.
How long does it take for muscle pain to go away after fixing thyroid levels?
Most people notice improvement within 4-6 weeks after their levothyroxine dose is adjusted and TSH starts to drop. Full recovery can take up to 12 weeks, especially if muscle damage was significant. If pain persists beyond that, other causes should be investigated.
Can I take CoQ10 instead of adjusting my thyroid meds?
No. CoQ10 may help reduce muscle discomfort, but it doesn’t fix the underlying issue - excess statin levels and poor muscle energy production caused by low thyroid hormone. Relying on CoQ10 alone is like using a flashlight to find your keys while the power’s still out. Fix the root cause first.
Is it safe to restart a statin after stopping it due to muscle pain?
Yes - if your thyroid function is optimized. Many patients who stopped statins because of muscle pain can safely restart them after their TSH is brought into the target range. Switching to a safer statin like rosuvastatin also improves success rates. Always restart under medical supervision with a baseline CK test.
What TSH level is too high to start a statin?
Experts recommend delaying statin initiation if TSH is above 7.0 mIU/L. At this level, the risk of myopathy rises sharply, and the benefit-risk balance becomes questionable. The goal is to treat hypothyroidism first, get TSH below 4.0, and ideally between 0.5 and 3.0, before starting or continuing statins.
Do I need to check CK levels regularly if I’m on both medications?
Yes. Get a baseline CK test before starting a statin. Then check again at 3 months and whenever you develop new muscle pain, weakness, or dark urine. CK levels above 10 times the upper limit of normal, or above 5 times with symptoms, usually mean you need to stop the statin and reevaluate your thyroid treatment.





Reviews
Okay but have you ever considered that Big Pharma is quietly pushing statins because they know thyroid patients are vulnerable? They don't want you to fix your thyroid-they want you to keep buying pills. CoQ10 is banned in 14 countries for a reason. The FDA’s new guidance? A distraction. They’re covering for the real issue: statins were never meant for people with metabolic dysfunction. You’re being manipulated.
And don’t even get me started on how they label TSH ‘normal’ at 4.0. That’s a corporate number. Real normal is under 2.0. I’ve seen it. I’ve lived it. And no, I won’t take your ‘evidence’-I’ve read the raw data.
They’re lying to you. All of it.
And yes, I’m on rosuvastatin. Still scared.
There’s something deeply human here. We treat medicine like a switch-on or off, fix or fail. But the body isn’t a machine. Hypothyroidism isn’t just a lab value. It’s a whisper of systemic imbalance. And statins? They’re blunt instruments in a symphony that’s already out of tune.
Maybe the real question isn’t which statin is safest-but whether we’re treating the whole person, or just the numbers we can measure.
I’ve seen people stop statins, optimize thyroid, and feel like themselves again. Not because of drugs, but because they finally listened to their body’s quiet screams. That’s not medicine. That’s reconnection.
Oh my god. This is the most important thing I’ve read this year. I’m not even on statins but I have Hashimoto’s and I just had a 4-hour panic attack because I thought my leg cramps were ‘just aging’-turns out my TSH was 7.8. I didn’t even know that was a thing.
I just called my endo. She said ‘we’ll adjust your dose’ like it’s Tuesday. I cried. Not from sadness-from relief. This isn’t just medical advice. It’s a lifeline.
Also-rosuvastatin? I’m switching. No more simva. No more nightmares. I’m 42. I want to hike with my kids. Not lie on the couch wondering if my muscles are dying.
OMG I’ve been feeling this for YEARS 😭 I was like ‘why am I so weak??’ and my dr just said ‘you’re getting older’ 🙄 I was on simva 40mg and my CK was 18k 😳 I thought I was gonna die. Switched to rosuvastatin 10mg, got my TSH down to 1.9, and now I can carry groceries without crying. THANK YOU for writing this. I’m sharing this with EVERYONE. 🙏❤️
Most people don’t realize how much thyroid affects everything. It’s not just fatigue or weight. It’s your mitochondria. It’s your liver. It’s your muscle repair. Statins are like pouring gasoline on a slow-burning fire. You don’t fix the fire-you just add more fuel.
If you’re on levothyroxine and still having muscle pain, your TSH isn’t optimized. It’s not ‘side effect.’ It’s a red flag. Get tested. Don’t wait. Don’t assume you’re fine. Your body is screaming. Listen.
And if your doctor says ‘it’s just statin myopathy’ without checking TSH? Find a new doctor. Seriously. This isn’t optional. This is basic.
bro i just found out my tsh was 8.2 last month and i was on atorvastatin 20mg and i thought i was just lazy lol. switched to rosuvastatin 10mg and bumped my levothyroxine to 112 mcg. 3 weeks later i could lift weights again. i was like ‘wait… i used to be strong?’
coq10? yeah i take it but its like putting air in a flat tire that still has a nail in it. fix the nail first. thyroid first. statin second.
also i think the docs dont check tsh because they dont wanna admit they missed it. its easier to say ‘oh statins cause pain’ than ‘we forgot to treat your thyroid.’
This is the kind of post that makes me believe in medical communities again. I’m from Nigeria, and here, most people don’t even know what TSH is. I’ve seen friends with hypothyroidism on statins, suffering, and told to ‘just take painkillers.’
I shared this with my cousin. She’s 56, on simvastatin, TSH 9.1. She cried when she read it. She’s getting tested tomorrow. Thank you. This isn’t just science. It’s dignity.
While the sentiment is well-intentioned, the presentation is alarmist and lacks the requisite scholarly restraint. One cannot, in good scientific conscience, reduce complex pharmacokinetic interactions to a binary of 'fix thyroid or die.' The cited studies, while compelling, are observational and subject to selection bias. Moreover, the endorsement of rosuvastatin as a panacea ignores the emerging evidence of its renal and metabolic consequences in elderly populations. To suggest that 85-90% of patients can safely remain on statins after thyroid optimization is an overgeneralization unsupported by longitudinal data. This is not education-it is therapeutic activism masquerading as clinical guidance.