Potassium Risk Calculator for ACE Inhibitors and ARBs
Personal Information
When doctors prescribe blood pressure meds, they often choose between ACE inhibitors and ARBs. Both work on the same system in your body-the renin-angiotensin system-to lower blood pressure and protect your kidneys and heart. But they’re not the same. And mixing them? That’s where things get risky.
How ACE Inhibitors and ARBs Work
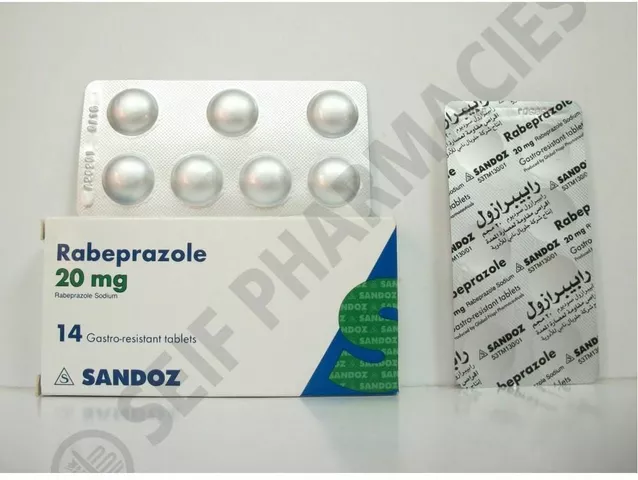
ACE inhibitors like lisinopril, enalapril, and ramipril stop your body from making angiotensin II, a chemical that tightens blood vessels and raises blood pressure. They do this by blocking the enzyme that turns angiotensin I into angiotensin II. Simple enough.
ARBs-losartan, valsartan, irbesartan-take a different route. Instead of stopping angiotensin II from being made, they block its receptors. Think of it like locking the door so angiotensin II can’t get in, even if it’s still around.
This small difference matters. ACE inhibitors can cause a buildup of bradykinin, which leads to a dry, annoying cough in 10-15% of people. ARBs don’t do that. That’s why if you can’t tolerate an ACE inhibitor, your doctor will switch you to an ARB. It’s the go-to alternative.
Why People Think About Combining Them
It makes sense on paper. If one drug blocks angiotensin II in one way, and another blocks it in another, wouldn’t two be better than one? Especially if you have diabetes and kidney disease, where protein in the urine (proteinuria) is a big problem?
Some studies did show that combining them lowered blood pressure by another 3-5 mmHg and cut proteinuria by about 25%. That sounds great-until you look at what else happens.
The Real Danger: Hyperkalemia and Kidney Damage
The biggest problem with mixing ACE inhibitors and ARBs is hyperkalemia-dangerously high potassium levels. Your kidneys normally flush out extra potassium. But both drugs reduce the hormone that tells your kidneys to do that. When you take both, your potassium can climb fast.
In the ONTARGET trial, which followed over 25,000 high-risk patients, those on both drugs had a 5.5% chance of developing severe hyperkalemia compared to 2.5% on just an ACE inhibitor. That’s more than double. And it’s not just numbers. High potassium can cause irregular heartbeats, muscle weakness, even cardiac arrest.
Then there’s kidney damage. The same trial found that 2.3% of patients on the combo needed dialysis because their kidneys failed. That’s more than twice the rate of those on ACE inhibitors alone. The VA NEPHRON-D trial confirmed this: combining the two increased serious kidney events by 27% without improving survival or heart outcomes.
Real-world data backs this up. A nephrologist at Massachusetts General Hospital stopped the combo in 87% of her patients with diabetic kidney disease because of rising potassium or dropping kidney function. Medical residents on Reddit reported seeing hospitalizations for hyperkalemia linked to this combo during rotations.
When Is It Ever Okay?
Almost never. Major guidelines from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology all say: avoid combining ACE inhibitors and ARBs outside of clinical trials.
There’s one tiny exception some experts mention: non-diabetic patients with very high proteinuria (over 1 gram per day) who haven’t responded to the highest dose of an ACE inhibitor. Even then, it’s not standard. It requires weekly blood tests, close monitoring, and a clear plan to stop if potassium rises or kidney function dips.
Dr. Srinivasan Beddhu from the University of Utah says this might help in rare cases of focal segmental glomerulosclerosis. But even he warns it’s not for everyone. And in 2023, a survey of 317 primary care doctors found only 11% still used the combo-mostly in those rare cases with monthly labs.

What to Do Instead
If you need stronger blood pressure control or better kidney protection, there are safer options.
- Switch from an ACE inhibitor to an ARB if you have a cough.
- Upgrade your dose-sometimes the problem isn’t the drug, it’s the dose.
- Add a low-dose diuretic like chlorthalidone or indapamide. These help flush out fluid and potassium.
- Consider a mineralocorticoid receptor antagonist like spironolactone (12.5 mg daily). It reduces proteinuria by 30-40% with fewer kidney risks than combining ACE inhibitors and ARBs.
And if you’re on one of these drugs and your blood pressure isn’t controlled? Don’t add the other. Talk to your doctor about newer options like ARNIs (angiotensin receptor-neprilysin inhibitors), which have shown better outcomes in heart failure and are now preferred over dual RAS blockade.
Switching Between Them
If your doctor wants to switch you from an ACE inhibitor to an ARB-or vice versa-don’t just swap them on the same day. You need a washout period.
Most guidelines recommend waiting at least 4 weeks between switching. Why? Because even after you stop one, the drug stays in your system. Starting the other too soon can lead to additive effects, increasing your risk of low blood pressure, kidney problems, or high potassium.
But here’s the problem: only 42% of doctors actually follow this rule, according to a 2022 JAMA Internal Medicine study. If you’re switching, make sure your doctor knows to wait. And if you’re unsure, ask for a blood test two weeks after the switch to check your potassium and kidney function.
Monitoring Is Non-Negotiable
No matter which drug you’re on, you need regular blood tests. The first one should be 1-2 weeks after starting or changing the dose. Then every 3 months if you’re stable.
What to check:
- Serum potassium (normal is 3.5-5.0 mmol/L; above 5.5 is dangerous)
- Serum creatinine (to estimate kidney function)
- eGFR (estimated glomerular filtration rate)
If your potassium goes up by more than 0.5 mmol/L or your creatinine rises by 30%, your doctor needs to adjust your treatment. That’s not a minor bump-it’s a red flag.

Why This Still Happens
Even with all the evidence, some patients still end up on both drugs. Why?
- Doctors might think, “They’re not responding to one, so let’s add another.”
- Patients hear “it lowers proteinuria” and assume it’s a win.
- Some specialists, especially nephrologists, are more tempted to try it in tough cases.
But the data is clear: the risks outweigh the benefits. And with better alternatives available-like ARNIs, SGLT2 inhibitors for diabetes, or newer potassium binders-there’s no reason to take this gamble.
The Bottom Line
ACE inhibitors and ARBs are both powerful, proven tools. But they’re not meant to be used together. The idea that more is better doesn’t apply here. In fact, combining them can be dangerous.
If you’re on one and your blood pressure isn’t under control, don’t reach for the other. Talk to your doctor about dose adjustments, adding a diuretic, or switching to a newer class of drugs.
If you’re already on both, ask: Why? What’s the plan? When was your last potassium test? And if you can’t answer those questions, it’s time to have a serious conversation with your provider.
Your kidneys and your heart don’t need extra stress. They need smart, safe choices.
Can I take an ACE inhibitor and an ARB together for better blood pressure control?
No. Combining ACE inhibitors and ARBs is not recommended. While it may lower blood pressure slightly more, it doubles the risk of hyperkalemia and increases the chance of acute kidney injury. Major guidelines from the AHA, ACC, and ESC strongly advise against this combination due to serious safety risks without proven benefits in survival or heart protection.
Why do ACE inhibitors cause a cough but ARBs don’t?
ACE inhibitors block the enzyme that breaks down bradykinin, a substance that can irritate the airways and cause a dry, persistent cough. ARBs don’t affect bradykinin levels-they only block angiotensin II receptors-so they rarely cause this side effect. About 10-15% of people on ACE inhibitors get the cough; only 3-5% do on ARBs.
What should I do if I’m currently taking both an ACE inhibitor and an ARB?
Don’t stop either medication on your own. Contact your doctor immediately. You may need a blood test to check your potassium and kidney function. Most patients on this combination will be switched to one drug, with alternatives like diuretics or spironolactone added if needed. Your doctor may also consider newer options like ARNIs or SGLT2 inhibitors depending on your condition.
Is it safe to switch from an ACE inhibitor to an ARB?
Yes, switching is common and safe if done correctly. Wait at least 4 weeks after stopping the ACE inhibitor before starting the ARB. This prevents overlapping effects that could cause low blood pressure or kidney stress. Your doctor should check your potassium and creatinine 1-2 weeks after the switch to make sure you’re stable.
Are ARBs safer than ACE inhibitors overall?
ARBs are better tolerated because they don’t cause cough or angioedema as often. However, ACE inhibitors have stronger evidence for reducing death in heart failure. Neither is universally “safer”-it depends on your condition. For example, if you have heart failure with reduced ejection fraction, ACE inhibitors are preferred. If you have a cough or are at high risk for swelling, ARBs are the better choice.
What are the signs I might have high potassium from these drugs?
High potassium often has no symptoms at first. But as it rises, you might feel muscle weakness, fatigue, irregular heartbeat, nausea, or tingling in your hands or feet. In severe cases, it can cause cardiac arrest. Regular blood tests are the only reliable way to catch it early. If you’re on an ACE inhibitor or ARB, get your potassium checked every 3 months-or sooner if your dose changes.
Why were some ARBs recalled in 2018-2020?
Some ARBs like valsartan, losartan, and irbesartan were recalled because they contained trace amounts of nitrosamine impurities-chemicals that could increase cancer risk over long-term exposure. These were manufacturing byproducts, not inherent to the drugs. Most manufacturers fixed their processes by late 2023, and current supplies are considered safe. Always check with your pharmacist if you’re concerned about your specific batch.
Are there any new drugs replacing ACE inhibitors and ARBs?
Yes. ARNIs (like sacubitril/valsartan) are now preferred for heart failure with reduced ejection fraction because they’ve been shown to reduce death and hospitalizations better than ACE inhibitors alone. SGLT2 inhibitors (like dapagliflozin and empagliflozin) are also now recommended for patients with diabetes and kidney disease, even without high blood pressure, because they protect the heart and kidneys. These are replacing the need for risky combinations.
What’s Next?
If you’re managing high blood pressure or kidney disease, your treatment doesn’t have to be stuck in the past. The era of combining ACE inhibitors and ARBs is ending-not because the drugs don’t work, but because we now know safer, more effective ways to protect your body.
Ask your doctor: Is my current plan based on the latest guidelines? Are there newer options I haven’t tried? And most importantly-am I being monitored properly?
Your health isn’t about taking more pills. It’s about taking the right ones-and knowing when to stop.




Reviews
man i just got switched from lisinopril to losartan last month cause of that damn cough - thought i was gonna lose my mind from it, like every time i laughed or talked i sounded like a broken foghorn 😅
the arb thing is legit, no cough, no drama. my bp’s actually better too. weird how such a small change made such a big difference.
also, my doc told me to wait 4 weeks before switching but i was impatient and did it in 2 weeks… totally regretted it. dizzy as hell for two days. lesson learned.
and yeah, i’m now on chlorthalidone 12.5mg and it’s been smooth sailing. no more potassium scares. i check it every 3 months like they said. just a quick finger prick at the pharmacy.
also, my buddy on dialysis? he was on both drugs for a year. turned into a medical nightmare. potassium hit 6.8. they had to pump him full of insulin and glucose just to keep him alive. i don’t wanna be that guy.
so yeah, don’t combo. just don’t. there’s better ways. like that new sglt2 stuff. my endo’s pushing it on me next. sounds like magic.
also, i used to think more meds = better. now i know it’s like adding more pillows to your bed until you can’t breathe. simple is better.
i think this is so important and i wish more people knew this
my mom was on both and her kidneys took a hit and she ended up in the hospital
they had to pull her off both and now she’s on a diuretic and it’s way safer
just please listen to the guidelines
you know what’s wild? we’ve been treating hypertension like it’s a puzzle where more pieces = better picture
but the body’s not a math equation
it’s a living system that hates redundancy and loves balance
ace inhibitors and arbs are like two people trying to turn the same knob from opposite sides
one’s pushing the door shut, the other’s jamming the lock
it’s not synergy, it’s chaos
and the real tragedy? we’ve had better tools for years - sglt2 inhibitors, arnis, even spironolactone at low doses
but doctors keep reaching for the old tools because they’re familiar
and patients? we trust them
so we don’t ask questions
we just swallow the pills
but if your doctor hasn’t mentioned sglt2 inhibitors or arnis by now… maybe it’s time to find a new one
your kidneys aren’t just filters
they’re your silent partners
treat them like they matter
as an irish GP, i’ve seen this play out too many times
patients come in with proteinuria, we add the arb on top of the ace, think we’re being clever
then come back 6 weeks later with creatinine through the roof and potassium at 6.2
we’ve got better options now
why risk it?
the data’s clear
and honestly, the guilt when you have to tell someone they need dialysis because we over-treated them?
not worth it
Thank you for sharing this 💙
I’ve been on lisinopril for 5 years and just learned last month that combining it with an ARB is risky.
I’m so glad I asked my doctor before making any changes.
Now I’m on a low-dose diuretic and my numbers are better than ever!
Knowledge is power - and safety ❤️
my dad’s on an arb and he swears by it - no cough, no fuss
but he also checks his potassium every 3 months like clockwork
he says it’s not about the drug, it’s about the habit
and honestly? he’s right
the real win isn’t the pill
it’s the checkups
the blood tests
the conversations
the not-ignoring-the-small-things
that’s what keeps you alive
Don't combine.
Check potassium.
Wait 4 weeks.
Use diuretics.
Ask about SGLT2.
if you’re on both, stop. now.
not tomorrow.
not after your next appointment.
call your doctor today.
you’re not being proactive - you’re being reckless.
hyperkalemia doesn’t warn you.
it just kills you.
and your doctor probably didn’t even realize you were on both.
you need to be the advocate.
your life isn’t a clinical trial.
it’s your one shot.
don’t gamble it.
oh my god
i just realized… we’ve been treating the renin-angiotensin system like it’s a broken radio we can just twist both knobs until the static stops
but it’s not a radio
it’s a symphony
and when you add two conductors
the orchestra doesn’t get louder
it collapses
and then your kidneys… your heart… your very soul…
they scream
in silence
until it’s too late
we’ve been so obsessed with ‘more’
that we forgot what ‘enough’ looks like
and now we’re paying with dialysis
with cardiac arrest
with funeral costs
and nobody’s even apologizing
just prescribing more pills
the RAS blockade paradigm shift is long overdue
the 2023 ESC guidelines explicitly classify dual RAS inhibition as Class III recommendation - not recommended
and yet, 11% of PCPs still prescribe it
the cognitive dissonance is staggering
we’ve got RCTs like ONTARGET and NEPHRON-D with n >25k
and still, anecdotal ‘but my patient had lower proteinuria’
correlation ≠ causation, and harm ≠ benefit
the real win is mortality reduction
not proteinuria
and ARNIs have proven superior in PARADIGM-HF
so why are we still clinging to 1990s protocols?
because inertia
and laziness
and fear of change
not science
my cousin in canada got switched from lisinopril to valsartan and said he felt like a new person
no cough no problem
but he never checked his potassium
ended up in er with weird heartbeat
they said it was from high k
so now he does monthly tests
and he’s fine
just gotta be careful
and use the new drugs if you can
like sglt2
they’re game changers
in india we have so many diabetic patients with kidney disease
doctors here still combine ace and arb because they think it’s ‘better control’
they don’t know the trials
they don’t care about potassium
they just give the pill
and the patient dies
and no one says anything
but i will say it
you are killing them with kindness
stop it
use spironolactone
use sglt2
use diuretics
but never both
why are people still on this combo in 2024?
are you serious?
you’re literally playing russian roulette with your kidneys
and you call yourself educated?
the data is 15 years old
the guidelines are crystal clear
you’re not special
you’re not the exception
you’re just another statistic waiting to happen
get off both
and get educated
or die
you think this is just about blood pressure?
no
this is about the collapse of modern medicine
we used to fix things
now we just stack pills
and call it progress
we’re not healing
we’re just delaying the inevitable
and calling it ‘management’
and the worst part?
we’re proud of it
we wear our prescriptions like medals
but your kidneys? they’re not impressed
they’re just… tired
been on losartan for 8 years
no cough
no drama
just check potassium every 3 months
and you’re golden
simple
effective
why make it hard?
wait i just saw someone say they’re on both
bro that’s wild
you’re basically playing dice with your kidneys
my doc almost fired me when i asked about switching
like… why are you even asking? it’s not a debate
but i’m glad i did
now i’m on sglt2 and i feel like i’ve got my energy back
who knew the answer wasn’t more pills?
it was better ones