What Exactly Is Allergic Asthma?
Most people with asthma have the allergic kind. About 60% of the 25 million Americans with asthma are affected by it, according to the American College of Allergy, Asthma, and Immunology. This isn’t just regular asthma-it’s asthma that flips on when your immune system overreacts to things like pollen, dust mites, or cat dander. Your body treats these harmless substances like invaders, releasing chemicals that swell your airways, tighten your lungs, and make breathing hard. It’s not just about feeling stuffy. It’s about wheezing, coughing at night, and sudden attacks that can land you in the ER.
What makes allergic asthma different from other types? For one, it usually starts young. The average age of diagnosis is 12.3 years. If your parents or siblings have allergies or asthma, your risk goes up significantly. Blood tests often show high levels of IgE antibodies-sometimes over 100 kU/L-and skin prick tests will light up when exposed to specific allergens. If your sputum has more than 3% eosinophils (a type of white blood cell), that’s another clue your asthma is driven by allergy.
Top Triggers You Can’t Ignore
Not all triggers are the same. Some come and go with the seasons. Others live in your home, quietly causing problems every day.
- Tree pollen: Peaks in March. In many parts of the U.S., you’ll see 10-20 grains per cubic meter of air. Even low counts can trigger symptoms in sensitive people.
- Grass pollen: Hits hard in June. Counts can jump to 50-100 grains/m³. Mowing the lawn? That’s a red flag.
- Ragweed: The fall villain. September is peak season. Pollen counts can exceed 100 grains/m³, and thunderstorms make it worse-spores burst open in wet air, spreading even more.
- Dust mites: These microscopic bugs live in bedding, carpets, and upholstered furniture. They thrive where humidity is above 50%. The allergen they produce (Der p 1) is found in 84% of U.S. homes with high humidity. Just 2 µg per gram of dust is enough to trigger reactions.
- Cat dander: The protein Fel d 1 sticks to clothes, walls, and furniture. It’s in 79% of U.S. homes-even if you don’t own a cat. Levels above 8 µg/g are enough to cause symptoms.
- Mold: Alternaria mold spores spike in late summer. When counts go over 500 spores/m³, emergency room visits for asthma jump 3.5 times.
And don’t forget air pollution. Tiny particles from car exhaust or smoke (PM2.5) damage the lining of your airways, making it easier for allergens to sneak in. One study showed exposure to PM2.5 increases airway permeability by 40-60% in just 24 hours.
How to Actually Avoid Allergens (Not Just Guess)
Avoiding triggers isn’t about buying a fancy air purifier and calling it a day. It’s about consistent, measurable actions backed by science.
- Bedding: Swap out regular pillows and mattress covers for allergen-proof ones made of tightly woven fabric (look for a pore size under 10 microns). Brands like AllerZip Pro have been tested to reduce dust mite exposure by over 90%. Wash sheets weekly in water hotter than 130°F.
- Humidity: Keep indoor humidity between 30% and 50%. Use a hygrometer to check. Too high? Get a dehumidifier. The AprilAire 500M cuts humidity fast and reduces dust mite levels from 20 µg/g to less than 0.5 µg/g.
- Vacuuming: Use a vacuum with a HEPA filter. Do it at least twice a week. A 2021 study found this reduces cat allergen in carpets by 42%. Avoid feather dusters-they just kick allergens into the air.
- Pollen: On high-pollen days (check the National Allergy Bureau app), keep windows closed. Wear an N95 mask when doing yard work. Shower and change clothes right after coming inside-this cuts allergen transfer to your bedding by 70%.
- Cats: If you’re allergic and can’t part with your cat, keep it out of the bedroom. Wash your hands after petting it. Use a HEPA filter in the room where the cat spends most time. It won’t eliminate allergens, but it helps.
One Reddit user, after months of strict dust mite control, saw their peak flow jump from 380 to 470 L/min. That’s not magic. That’s science.
Immunotherapy: The Only Treatment That Changes the Course
Medications like inhalers and antihistamines treat symptoms. Immunotherapy is the only option that can actually change how your immune system responds to allergens.
There are two main types:
- Subcutaneous Immunotherapy (SCIT): Also called allergy shots. You get weekly injections for 4-6 months, slowly building up to a maintenance dose. Then you switch to monthly shots for 3-5 years. About 70-80% of people see major improvement after 12-18 months. A 2021 Cochrane review found it cuts asthma medication use by up to 40%.
- Sublingual Immunotherapy (SLIT): Daily tablets or drops placed under the tongue. Grastek (for grass) and Odactra (for dust mites) are FDA-approved. It’s less invasive, but side effects like mouth itching are common-78% of users report it in the first month. Still, 65% of users stick with it because it’s convenient.
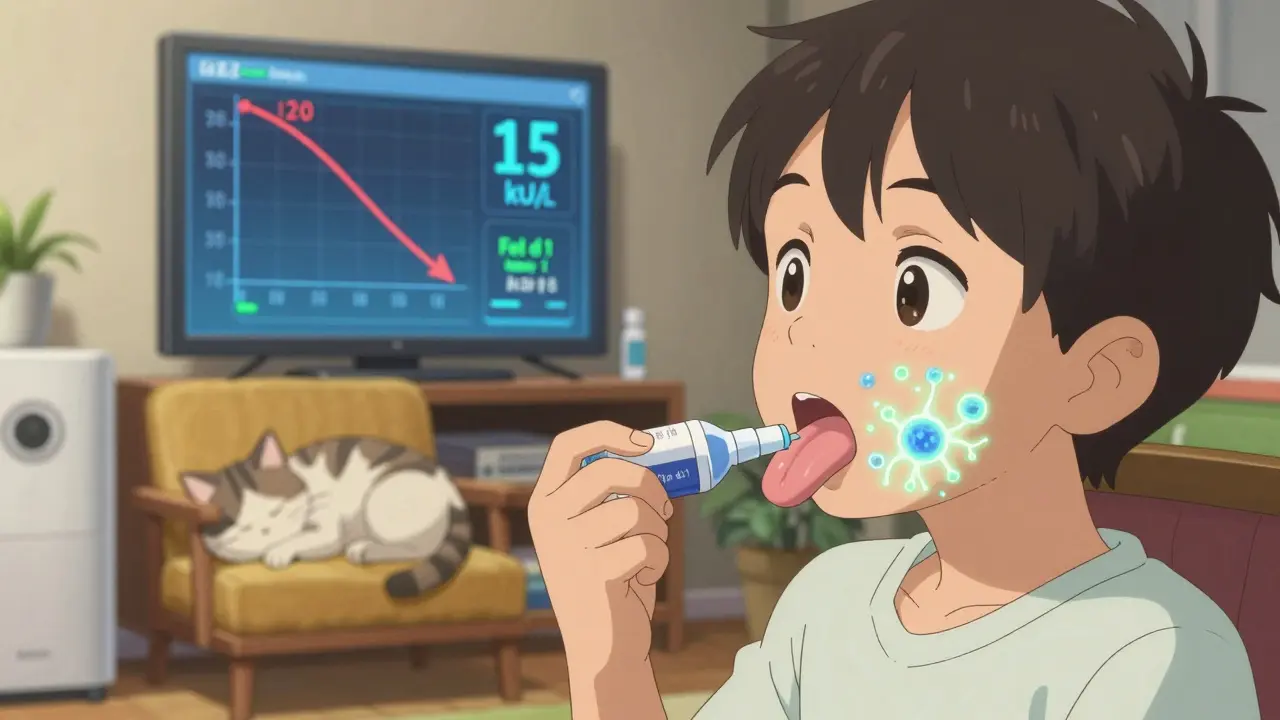
One standout case: a 12-year-old with severe cat allergy had a skin test wheal of 15mm. After three years of cat dander immunotherapy, their IgE dropped from 120 kU/L to 15 kU/L. Their symptoms vanished. They passed a challenge test-meaning they could now be around cats without reacting.
But immunotherapy isn’t for everyone. It takes time, money, and commitment. Medicare covers 80% of shots, with a $18.90 copay per injection in 2024. But out-of-pocket costs for SLIT can hit $200-$400 a month without insurance.
Why Some People Don’t Respond-And What to Do About It
Not everyone with allergic asthma has type 2 inflammation. That’s the immune pathway that responds to biologics like omalizumab or to immunotherapy. Studies show over 30% of people diagnosed with allergic asthma based on symptoms actually have non-type 2 inflammation. That means they’re getting expensive treatments that won’t help.
Doctors now use two key biomarkers to confirm:
- Blood eosinophils: Above 300 cells/µL? Likely type 2.
- FeNO (fractional exhaled nitric oxide): Above 25 ppb? Strong indicator of allergic inflammation.
If these markers are normal, your asthma might be triggered by something else-like cold air, stress, or pollution. In those cases, immunotherapy won’t work. You might need bronchial thermoplasty or low-dose macrolide antibiotics instead.
That’s why testing matters. Don’t assume your asthma is allergic just because you have seasonal symptoms. Get tested properly.

What’s New in 2026?
The field is moving fast. New tools are making management smarter.
- Allergen Insight: A nasal sensor (FDA breakthrough device) that detects airborne allergens as low as 0.1 µg/m³ and sends alerts to your phone.
- AsthmaIQ: An AI platform launched in April 2024 that combines pollen forecasts, your personal exposure history, and medication logs to predict your next asthma flare-up-with 92% accuracy.
- CAT-PAD: A new peptide-based therapy for cat allergy that cuts the buildup phase from six months to just eight weeks.
- Pollen-VLP vaccine: A new experimental vaccine requiring only four doses per year. Early trials show 60% symptom reduction.
By 2030, experts predict molecular diagnostics will cut unnecessary immunotherapy by 30%. And combining biologics with immunotherapy could push disease control rates from today’s 50% to 75%-saving billions in healthcare costs.
When to See an Allergist
If you’re using your rescue inhaler more than twice a week, waking up at night with asthma symptoms, or missing work or school because of flare-ups, it’s time to see an allergist. They can:
- Confirm if your asthma is allergic with skin or blood tests
- Measure your IgE and eosinophil levels
- Recommend allergen avoidance tailored to your triggers
- Decide if immunotherapy is right for you
- Help you avoid costly, ineffective treatments
Don’t wait until you’re in the ER. Allergic asthma is manageable-not because you’re lucky, but because you know what to do.
Can you outgrow allergic asthma?
Some children do outgrow it, especially if their triggers are limited and they avoid exposure. But for many, allergic asthma persists into adulthood. Immunotherapy can change that course-studies show 30-50% of patients stay in remission for years after stopping treatment. It doesn’t guarantee you’ll never have symptoms again, but it reduces the chance dramatically.
Is immunotherapy safe for kids?
Yes. Both allergy shots and sublingual tablets are approved for children as young as 5. SLIT is often preferred for kids because it’s needle-free and can be done at home. Side effects are mild-mostly mouth itching or stomach upset. The benefits of preventing long-term lung damage and reducing steroid use far outweigh the risks.
Can air purifiers cure allergic asthma?
No. Air purifiers with HEPA filters can reduce airborne allergens by 50-80%, but they don’t eliminate dust mites from bedding or cat dander from furniture. They’re helpful as part of a bigger plan-not a standalone solution. The most effective strategy combines filtration, humidity control, and allergen-proof covers.
Do I need to get rid of my pet if I’m allergic?
Not necessarily. Many people keep their pets and still control symptoms with a combination of HEPA filters, frequent cleaning, keeping pets out of bedrooms, and immunotherapy. A 2022 study showed that pet owners who used allergen-proof bedding and vacuumed twice weekly reduced airborne cat allergen by 60%. If immunotherapy is an option, it can allow you to live with your pet safely.
How long until I feel better with immunotherapy?
Most people start noticing improvements after 6-12 months. Full benefits usually take 12-18 months. It’s not a quick fix. But if you stick with it for 3-5 years, you’re likely to see lasting results-even after treatment stops. The PAT study showed patients stayed symptom-free for over a decade after completing therapy.
Can I stop my inhaler if I start immunotherapy?
Never stop your controller inhaler without talking to your doctor. Immunotherapy reduces the need for medications over time, but it doesn’t work overnight. Many people reduce their dose gradually as symptoms improve. Your doctor will monitor your lung function and adjust your plan based on FeNO levels, peak flow, and symptom logs.
Are there natural remedies that work for allergic asthma?
There’s no strong evidence that herbs, essential oils, or dietary changes cure allergic asthma. Some people report feeling better with vitamin D or omega-3 supplements, but these don’t replace proven treatments. The only natural approach with solid backing is allergen avoidance-cleaning, humidity control, and reducing exposure. Everything else is unproven and can delay real treatment.






Reviews