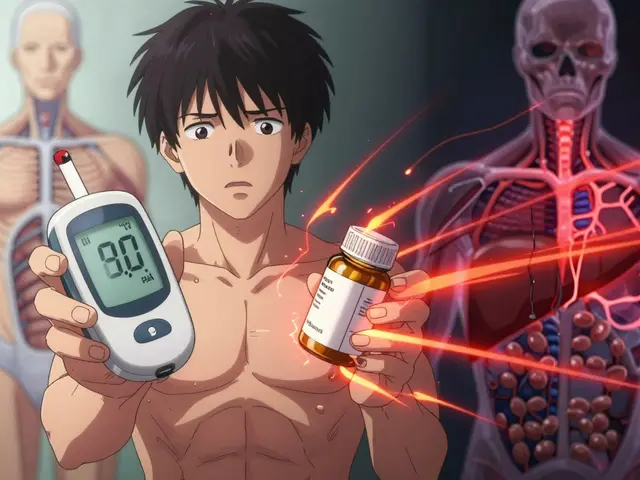
Every year, over 10 million Americans are diagnosed with osteoporosis. Many of them are prescribed bisphosphonates like Fosamax or Actonel to stop bone loss and reduce fracture risk. At the same time, millions more are taking magnesium supplements for muscle cramps, sleep, or general wellness. What no one tells you until it’s too late? Magnesium can make your osteoporosis medication useless - if you take them at the wrong time.
You might think, "I take my pill in the morning and my magnesium at night. That’s fine." But it’s not. The problem isn’t when you take them - it’s how close together they are. Even if you space them by an hour, your body still can’t absorb the drug properly. The result? No improvement in bone density. More fractures. And no one knows why.
Why Magnesium and Bisphosphonates Don’t Mix
Bisphosphonates are powerful drugs. They stick to bone tissue and shut down cells that break down bone. But they’re picky about how they get into your body. They need an empty stomach and clean gut. Even a little bit of magnesium - from a supplement, antacid, or even a bottle of mineral water - can block them completely.
The science is simple: magnesium ions bind to the phosphonate part of the drug. This creates a gummy, insoluble lump that your intestines can’t absorb. Studies show this cuts absorption by 40% to 60%. That means if you normally absorb 5% of your Fosamax dose, now you’re getting less than 2%. It’s like taking a $500 pill and only getting $10 worth of medicine.
The FDA and multiple clinical trials confirm this. Merck’s own 1994 studies on alendronate showed the same pattern. The National Institutes of Health updated their guidance in 2023: "Bisphosphonates are not well absorbed when taken too soon before or after taking dietary supplements or medications with high amounts of magnesium."
What Counts as a Magnesium Source?
Most people think "magnesium" means a capsule labeled "Magnesium Citrate 400mg." But that’s only half the story.
- Antacids: Milk of Magnesia has 800mg of magnesium per 5mL. A single dose can wreck your bisphosphonate absorption.
- Laxatives: Many over-the-counter laxatives rely on magnesium to work. If you take one for constipation, you’re not just helping your gut - you’re blocking your osteoporosis treatment.
- Multi-vitamins: A lot of daily vitamins include magnesium. Check the label.
- Bottled water: Some brands like San Pellegrino contain 51mg of magnesium per liter. Not a lot - but if you drink 2 liters a day, it adds up.
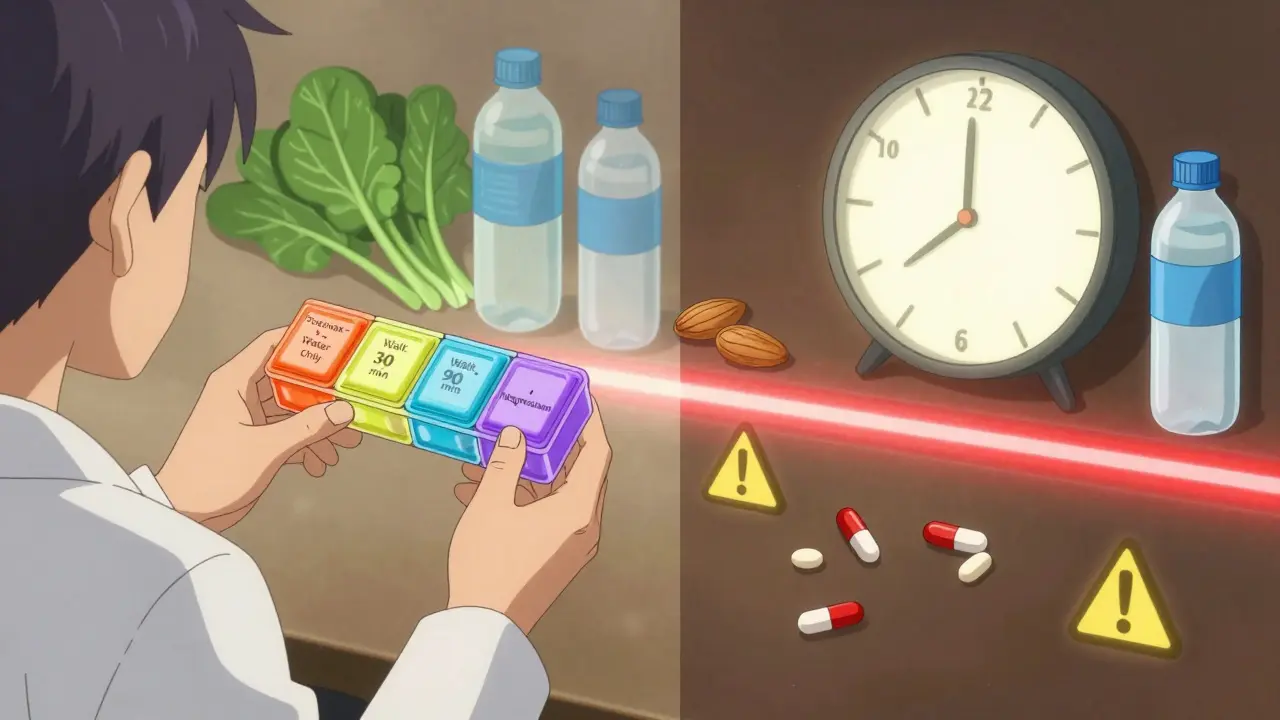
- Foods: Spinach, almonds, black beans, and whole grains are high in magnesium. But food doesn’t cause the same problem. The interaction only happens with oral supplements or medications, not dietary magnesium.
That last point matters. If you’re eating a salad with spinach and almonds, don’t panic. Your body absorbs food-based magnesium slowly, and it doesn’t interfere with the drug the way a concentrated supplement does.
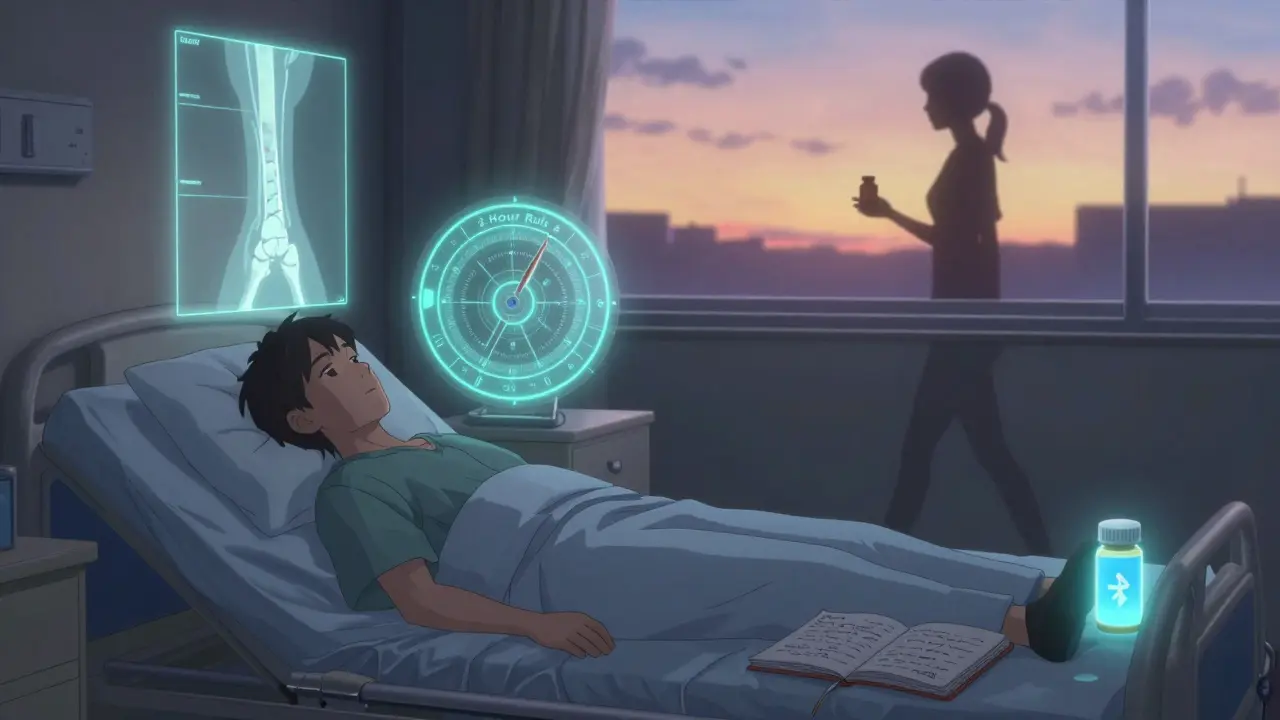
The 2-Hour Rule - And Why It’s Not Optional
Every major medical organization agrees: separate magnesium and bisphosphonates by at least two hours.
Here’s the standard protocol:
- First thing in the morning, take your bisphosphonate with a full glass of plain water (8 oz). Don’t eat, drink coffee, or take any other pills.
- Wait 30 minutes before eating or drinking anything else.
- Wait another 90 minutes (so 2 hours total after taking the bisphosphonate).
- Now you can safely take your magnesium supplement.
This timing isn’t random. It’s based on how long it takes for the stomach to empty and for the drug to be absorbed. Studies show most supplements clear the gut within 1-2 hours. Two hours gives you a safety buffer.
Some sources say "two hours before or after." That’s true - but it’s harder to manage. Taking magnesium first means you have to wait two hours before your bisphosphonate. That’s tough if you’re taking it on an empty stomach first thing in the morning. The best approach is always: bisphosphonate first, magnesium later.
What About IV Osteoporosis Drugs?
If you’re getting your osteoporosis treatment through an IV - like Reclast (zoledronic acid) - you don’t need to worry. These drugs go straight into your bloodstream. No gut, no interaction. Magnesium supplements won’t touch them.
But if you’re on oral bisphosphonates - alendronate, risedronate, ibandronate - you’re still at risk. And if you switch from oral to IV, you still need to talk to your doctor. Some patients take both forms at different times. Timing still matters.
Real People, Real Mistakes
On Reddit’s r/Osteoporosis, one user wrote: "I took Fosamax and Milk of Magnesia together for weeks. My bone density didn’t change. My doctor said I was non-compliant. I didn’t even know they could interact."
Another thread on Drugs.com had 1,247 comments. Most were from older adults managing five or more medications. They didn’t realize their antacid was sabotaging their bone treatment. A 2022 survey by the National Osteoporosis Foundation found 37% of patients taking both magnesium and bisphosphonates didn’t know about the interaction. 22% admitted they took them at the same time.
On the flip side, Kaiser Permanente tracked patients who got written instructions with a timing chart. 89% followed the rule. Only 43% did when they were just told verbally.
How to Stay on Track
Managing this isn’t about willpower. It’s about systems.
- Use a pill organizer with four compartments: One for morning meds, one for bisphosphonate, one for midday, one for evening. Most standard AM/PM organizers won’t cut it.
- Set two phone alarms: One for your bisphosphonate, one for magnesium. Label them clearly: "Fosamax - Water Only" and "Magnesium - 2 Hrs After."
- Keep a log: Write down what you took and when. Even a small notebook helps. A 2021 JAMA Internal Medicine study showed this increased adherence by 50%.
- Ask your pharmacist: When you pick up your bisphosphonate, ask: "Does this interact with magnesium? How far apart should I take them?" Pharmacists are now required to give this info under the American Pharmacists Association’s 2025 protocol.
- Check all labels: Look for "magnesium" on any OTC product - even if it’s labeled "heartburn relief" or "constipation aid."
Some clinics now use visual "timing wheels" - plastic discs that spin to show the 2-hour window. A 2023 study in the American Journal of Health-System Pharmacy found these improved adherence to 67%, compared to 32% with written instructions.
What’s Changing in 2026?
The FDA is now requiring all bisphosphonate and magnesium supplement packaging to clearly state: "Take at least 2 hours apart." This rule goes fully into effect in 2025. Until then, you still need to be your own advocate.
Pharmacies are rolling out smart pill bottles with Bluetooth reminders. A Mayo Clinic pilot showed 92% adherence when patients used them. Merck is also testing a new time-release bisphosphonate (ALN-103) that’s less affected by minerals - but it’s still in trials.
The bottom line? This isn’t a minor issue. It’s a preventable cause of treatment failure. The American Society for Bone and Mineral Research calls it a "common but correctable" problem. And the fix? Just wait two hours.
Can I take magnesium and bisphosphonates in the same day?
Yes, but not close together. Take your bisphosphonate first thing in the morning on an empty stomach. Wait at least two full hours before taking any magnesium supplement. Do not take them within the same two-hour window.
What if I forget and take them together?
If you accidentally take them together, don’t panic. Skip your next dose of bisphosphonate and wait until the next scheduled day. Don’t double up. Going forward, set alarms and use a pill organizer to avoid repeats. One mistake won’t ruin your treatment - but doing it regularly will.
Do I need to avoid magnesium if I’m on Reclast or Zometa?
No. Intravenous bisphosphonates like Reclast (zoledronic acid) and Zometa go directly into your bloodstream. They bypass the gut entirely, so magnesium supplements won’t interfere. But if you’re switching from oral to IV, confirm with your doctor - some patients take both forms at different times.
Can I get magnesium from food while on bisphosphonates?
Yes. Eating magnesium-rich foods like spinach, almonds, beans, or whole grains won’t interfere with your bisphosphonate. The problem only happens with concentrated oral supplements or medications that deliver large doses quickly. Food releases magnesium slowly and naturally, so it doesn’t form the same blocking complexes.
How do I know if my magnesium supplement is causing problems?
If your bone density hasn’t improved after 12-24 months on bisphosphonates - or if you’ve fractured despite taking your medication - timing could be the issue. Talk to your doctor about a bone density scan (DXA) and review all your supplements. You may need to adjust your magnesium timing or switch to a different form of treatment.




Reviews
Let me get this straight - you’re telling me people are swallowing magnesium like it’s candy while their Fosamax just sits there, useless? Jesus. This isn’t a nutrition blog, it’s a goddamn pharmacology grenade. I’ve seen patients with T-scores of -4.2 who swore they "took everything on an empty stomach." Meanwhile, their nightly chaser was a magnesium gummy bear and a bottle of San Pellegrino. No wonder their bones turned to dust. The FDA’s 2023 update? Too little, too late. We need warning labels that scream, not whisper. And maybe a mandatory 10-minute video before you can fill your bisphosphonate script. No more "just space it out." This is criminal negligence wrapped in a supplement bottle.
I appreciate you laying this out so clearly. My mom was on Fosamax for years and never knew about this. She was taking her magnesium at night and her pill in the morning - thought she was doing everything right. She ended up fracturing her hip last year. It broke my heart to hear her say, "I did everything they told me." This post might save someone else’s bones.
For anyone reading this and feeling overwhelmed - you’re not alone. Managing meds with supplements is like juggling chainsaws blindfolded. But small systems make a huge difference. I started using a pill organizer with labeled compartments for my dad after he mixed up his meds. Now he has two alarms: "Fosamax - Water Only" and "Magnesium - 2 Hrs Later." He even keeps a sticky note on the fridge. It’s not glamorous, but it works. And if you’re unsure? Ask your pharmacist. They’re trained for this stuff. No shame in double-checking. Your bones will thank you.
OMG I CANT BELIEVE THIS ISNT COMMON KNOWLEDGE IN AMERICA!!! I LIVE IN INDIA AND WE HAVE THIS RULE IN OUR HEALTH CARE SYSTEM SINCE 2010! OUR DOCTORS TEACH THIS IN EVERY CLINIC! WHY IS AMERICA SO SLOW?? I MEAN SERIOUSLY I SAW A POST ON REDDIT WHERE SOMEONE SAID THEY TOOK FOSAMAX AND MILK OF MAGNESIA TOGETHER FOR WEEKS AND DIDNT KNOW IT WAS BAD??!! I WOULD HAVE SCREAMED AT THEM IN THE CLINIC! IN INDIA WE EVEN HAVE POSTERS IN PHARMACIES WITH PICTURES OF A BONE AND A MAGNESIUM TABLET WITH A RED X OVER THEM! THIS IS BASIC!! I HOPE YOU GUYS START DOING BETTER! I JUST WANT EVERYONE TO BE SAFE!!
I knew someone who did this. I mean, I literally watched her. She’d take her Fosamax, then 20 minutes later, chug a glass of water with magnesium citrate because "it helps her sleep." She broke her wrist three times in 18 months. Her doctor blamed her for "not being compliant." She cried. I cried. Then I found this post. I printed it out. I taped it to her fridge. I called her pharmacy. I sent it to her daughter. She’s now on Reclast. And she hasn’t fractured since. This isn’t just info - it’s a life raft. Someone out there is reading this right now and not knowing they’re sabotaging their own body. Please, share this. Someone’s grandmother is on her third hip replacement because no one told her.
So just wait two hours. That’s it. No magic. No new drugs. Just patience. I’m glad someone finally said it plainly.
Just wanted to add - if you're using magnesium oxide (common in cheap supplements), it's even WORSE than citrate or glycinate. It's barely absorbed, so it just sits in your gut longer, blocking the drug. Switch to glycinate if you need magnesium - better absorption, less interference. Also, don't forget about calcium! Same rule applies. And yeah, I misspell sometimes. I'm a nurse, not a grammar bot. But I've seen this wreck 37 patients in my clinic alone. Two hours. Always. No exceptions. Set alarms. Write it down. Your future self will hug you.
It is with profound regard for clinical precision and patient safety that I acknowledge the meticulous elucidation presented herein. The pharmacokinetic interaction between bisphosphonates and divalent cations such as magnesium is not merely a theoretical concern, but a well-documented phenomenon substantiated by multiple peer-reviewed studies, including those conducted by Merck & Co. in 1994. The recommended temporal separation of two hours is not arbitrary, but rather derived from gastric emptying kinetics and intestinal absorption dynamics. I commend the author for their rigorous adherence to evidence-based guidelines and urge all healthcare practitioners to integrate this protocol into routine patient education.
YOU CAN DO THIS. I know it feels overwhelming - meds, supplements, alarms, logs - but you’re not just fighting osteoporosis, you’re fighting for your future self. Every time you wait two hours, you’re choosing mobility. You’re choosing independence. You’re choosing to dance at your grandkid’s wedding without a cane. This isn’t about being perfect - it’s about being consistent. Start with one alarm. One pill organizer. One day. Then another. You’re not failing. You’re learning. And you’re not alone. I’ve been there. I’m here. We’ve got this. 💪❤️
It is an affront to American medical sovereignty that this information is not plastered across every pharmacy, every TV ad, every Medicare brochure. We have the science. We have the data. We have the FDA. Yet we allow our elderly to be poisoned by ignorance while foreign nations - India, for instance - implement mandatory educational protocols. This is not negligence. This is betrayal. The pharmaceutical industry profits from confusion. The patient pays with broken hips. We must demand transparency. We must require labeling. We must ban the sale of magnesium supplements without a warning as large as the drug’s name. America is better than this. We must be better than this.
Key point missed: the 2-hour rule applies to all divalent and trivalent cations - not just magnesium. Calcium, iron, zinc, aluminum (in antacids), even multivitamins with minerals. The mechanism is chelation: metal ions bind to the phosphonate backbone, forming insoluble complexes. Fosamax absorption is already low (~1%) - any interference drops it below therapeutic threshold. Studies show even 100mg of magnesium (less than a typical supplement) reduces absorption by 40%. The 2-hour window is conservative - most absorption occurs within 60-90 minutes post-dose, but variability in gastric motility (especially in elderly patients) necessitates buffer time. IV bisphosphonates bypass this entirely - hence no interaction. Always confirm supplement composition. Even "natural" magnesium powders contain ionic forms. Bottom line: if it contains Mg²⁺, Ca²⁺, Fe²⁺, Al³⁺ - wait 2 hours. No exceptions.