When your kidneys fail, you don’t have to spend hours in a clinic three times a week. Peritoneal dialysis lets you treat yourself at home using your abdomen’s natural lining as a filter. It’s not one-size-fits-all. Two main methods exist: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD). Both work, but they change your life in very different ways.
How Peritoneal Dialysis Works
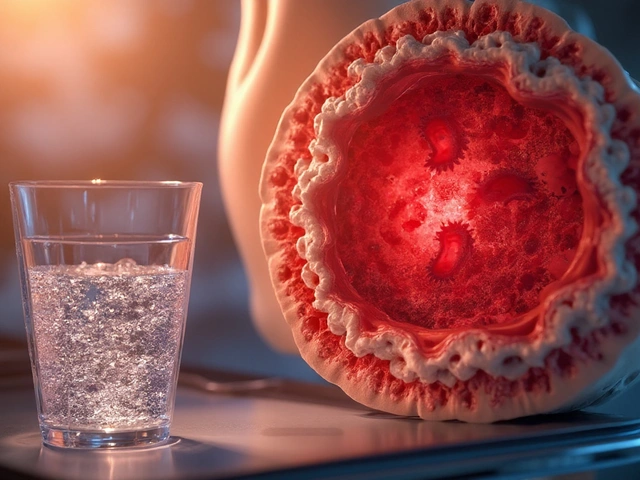
Every day, your kidneys clean about 200 quarts of blood. When they stop working, toxins and fluid build up. Peritoneal dialysis uses a soft tube (catheter) placed in your belly. A special fluid called dialysate flows in, pulls out waste and extra water, then drains out. It’s like a slow, steady rinse-no big machines needed for CAPD, just gravity and your hands. APD uses a machine to do the same thing while you sleep.
Both types use the same dialysate solutions-usually 1.5%, 2.5%, or 4.25% dextrose. The concentration determines how much fluid gets pulled out. Higher numbers mean more fluid removal, but they can also irritate the belly lining over time. You’ll need a clean space to do exchanges, and strict hygiene is non-negotiable. One mistake can lead to peritonitis, an infection that sends most people back to the hospital.
CAPD: Manual Exchanges, Full Control
CAPD has been around since the 1970s. It’s simple: you do 3 to 5 exchanges a day, each taking 30 to 40 minutes. You hang a bag of fluid, let it sit for 4 to 6 hours (called a dwell), then drain it into a collection bag. You can walk around during the dwell. No electricity. No machine. Just bags, tubing, and a clean surface.
People who choose CAPD often value freedom. A 58-year-old teacher in Ohio told me he does exchanges during his planning period between classes. No alarms. No setup. Just grab a bag from the closet, do the swap, and go. It’s portable. You can travel with it. Backpacks designed for dialysis bags exist. You can even do exchanges in a bathroom stall if needed.
But it’s not easy. Each exchange requires precise hand movements: connecting tubing, clamping lines, avoiding contamination. If your hands shake from arthritis or nerve damage, it’s tough. Around 38% of dialysis patients over 65 struggle with manual dexterity, according to USRDS data. That’s why some older patients drop out. And yes-you’re doing this 4 or 5 times a day, every day. No breaks. No vacations without planning.
Peritonitis risk is higher with CAPD. The USRDS 2021 data shows 0.68 episodes per patient-year, compared to 0.52 for APD. Why? More hand contact. More chances for bacteria to sneak in. Training takes 10 to 14 days. Nurses drill you on sterile technique until you can do it blindfolded. Still, mistakes happen.
APD: Sleep, Not Stress
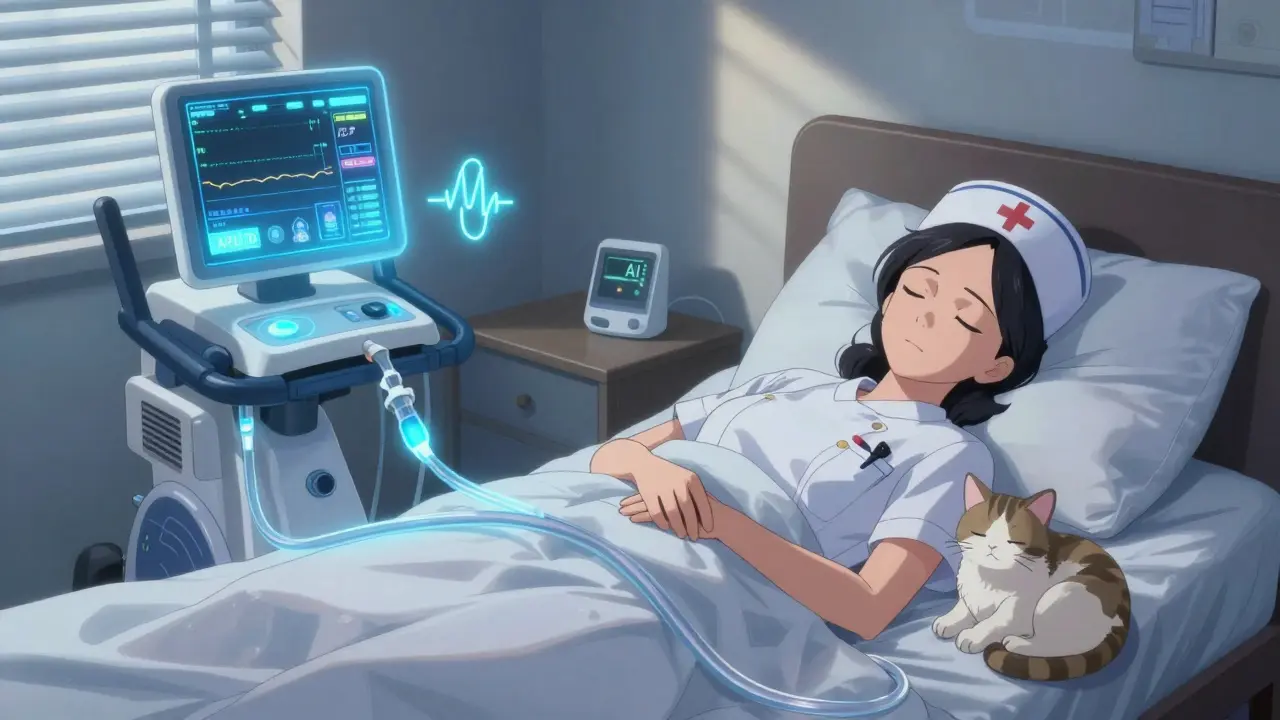
APD came along in the 1980s and got better every decade. Today’s cyclers-like the Baxter Amia or Fresenius Sleep-Safe-are smaller than a microwave, weigh 15 to 25 pounds, and run on a standard outlet. You hook up at night, press start, and sleep. The machine does 9 to 12 exchanges automatically while you rest. No daytime interruptions.
For working parents, shift workers, or anyone who hates being tied down during the day, APD is a game-changer. An ER nurse in Michigan, 42, says it lets her work 12-hour shifts without missing a beat. She doesn’t carry bags. She doesn’t plan lunch around a drain. She sleeps. And she gets 3.2 more hours of sleep per night than CAPD users, according to Mayo Clinic data.
But there’s a catch. Machines break. About 12% of APD users face a cycler malfunction each year. That means emergency calls, waiting for parts, or rushing to the clinic. One woman in Texas told me her machine died at 2 a.m. She had to do a manual exchange with a flashlight because the power was out. Not ideal.
Modern cyclers have safety features: air bubble detectors, pressure sensors, UV disinfection. Baxter’s Amia system even uses AI to adjust fluid removal based on your daily weight and blood pressure. In trials, it cut fluid overload events by 31%. Remote monitoring lets your care team see if you missed a cycle or had a leak-before you get sick. That’s huge. It reduces hospital visits by 25%.
Training takes longer: 14 to 21 days. You learn how to set up the machine, troubleshoot alarms, and clean the tubing. It’s more complex than CAPD, but once you’re used to it, your routine is predictable. You don’t have to think about it during the day.
Costs and Insurance
Medicare covers 80% of home dialysis costs in the U.S. The rest depends on your plan. CAPD supplies-bags, tubing, disinfectants-cost $50 to $75 a month. APD runs $75 to $100 because you’re renting the cycler. Some insurance plans cover the machine entirely. But here’s the twist: APD can lower your long-term costs. Better fluid control means fewer blood pressure meds, less hospitalization for heart failure, and fewer ER trips. One study showed APD users saved 15-20% on medications over five years.
Outside the U.S., countries like Germany and France pay more for APD to encourage its use. In rural America, access is still a problem. Only 32% of rural clinics offer full home dialysis training. If you live far from a center, you might not get the support you need-even if you’re a perfect candidate for APD.
Who Benefits Most?
There’s no universal answer. But patterns emerge.
- Choose CAPD if: You’re over 75, have limited space, travel often, or prefer total control without machines. You’re comfortable with routine manual tasks and have good hand coordination. You live where electricity is unreliable.
- Choose APD if: You’re under 65, work full-time, have trouble sleeping due to fluid buildup, or want fewer daytime disruptions. You have reliable power, space for the machine, and someone who can help with setup if needed. You’re tech-savvy enough to handle alarms and updates.
Dr. Michael J. Germain, a nephrologist at Baystate Medical Center, says CAPD is still the gold standard for patients over 75. Simpler. Fewer things to go wrong. But Dr. Beth Piraino from UPMC argues APD should be first-line for anyone under 65. The data supports her: better sleep, fewer hospitalizations, improved quality of life scores.
Here’s what’s surprising: APD users report 18% higher quality-of-life scores on surveys. But CAPD users are 22% more satisfied with travel flexibility. So if you love road trips, CAPD might win. If you hate being woken up by alarms? APD wins.

What No One Tells You
Both methods need a clean, quiet space. For CAPD, that’s a countertop. For APD, you need a 2x2 foot area near an outlet. And noise? Cyclers hum at 35 to 45 decibels-like a quiet library. But if you’re a light sleeper, even that can break your rest. Some patients use white noise machines. Others move the cycler to a closet or basement.
Storage matters too. You’ll need room for 4 to 6 dialysate bags at a time. That’s about 4x4 feet of space. If you live in a studio apartment, you might need to rearrange. Some patients store bags under the bed or in a closet.
And support? APD programs offer 24/7 technical help. CAPD? Not always. If your catheter leaks at 3 a.m., who do you call? Make sure your clinic has a real emergency line-not just a voicemail.
The Future Is Connected
By 2030, APD is expected to make up 65% of home dialysis. Why? Because tech keeps improving. New cyclers connect to smartphones. You can check your last exchange, get alerts, and even send data to your doctor without leaving your couch. The first FDA-approved smartphone-connected cycler is expected in 2025. It cuts setup errors by 40%.
And research is ongoing. The HOME-PD trial (2023-2026) is comparing long-term outcomes. Early results show APD users feel better, sleep better, and miss less work. But CAPD isn’t disappearing. It’s cheaper. Simpler. Vital for people without power, space, or tech access.
One thing’s clear: both work. But your life, your body, and your daily rhythm should decide which one fits.
Can I switch from CAPD to APD later?
Yes, you can switch. Many people start with CAPD because it’s simpler, then move to APD when they need more convenience or better sleep. Your care team will assess your catheter health, home setup, and ability to learn new tech before switching. It’s common and safe.
Do I need a caregiver for APD?
Not necessarily. Most people do APD alone. But if you have poor vision, limited mobility, or cognitive issues, having someone help with setup or troubleshooting is wise. Medicare now covers training for family members as care partners, so your spouse, child, or friend can learn how to help if needed.
Is APD noisy enough to disrupt sleep?
Modern cyclers are quiet-about 35 to 45 decibels, like a library. But if you’re a light sleeper, it can still bother you. Some users move the machine to another room and run the tubing under the door. Others use white noise machines or earplugs. If noise is a dealbreaker, CAPD might be better.
Which method has fewer infections?
APD has a lower peritonitis rate: 0.52 episodes per patient-year versus 0.68 for CAPD. Why? Fewer manual exchanges mean fewer chances for bacteria to enter. APD also uses closed-system tubing and built-in disinfection. Still, hygiene matters more than the method. Wash your hands. Keep your space clean. That’s the real key.
Can I still work full-time with either option?
Absolutely. CAPD users often exchange during breaks or lunch. Many employers are legally required to accommodate dialysis schedules. APD users rarely interrupt their day-they treat while they sleep. About 65% of CAPD users and 55% of APD users maintain full-time jobs. APD gives you more flexibility for irregular hours or shift work.