Drug-Supplement Interaction Checker
Enter your prescription or over-the-counter medications (e.g., warfarin, metformin, levothyroxine)
Enter supplements you take (e.g., vitamin K, St. John's wort, magnesium)
Every year, millions of people in the U.S. take supplements alongside prescription or over-the-counter meds-without knowing they might be putting their health at risk. You might think if it’s on the shelf at the grocery store, it’s safe. But that’s not true. Supplement labels don’t tell you the full story. Unlike pills from your pharmacist, supplements aren’t required to warn you about dangerous interactions with your medications. And that gap? It’s deadly.
What You’ll Find on a Supplement Label (and What’s Missing)
Start with the Supplement Facts panel. It looks like a nutrition label. It shows serving size, how much of each ingredient is in one dose, and the % Daily Value. But here’s the catch: if it says proprietary blend, you’re in the dark. That means the manufacturer won’t tell you how much of each ingredient is actually in there. One protein powder I checked had six different herbs in a blend-but no amounts. You can’t know if you’re getting enough-or too much.
Look for allergens. The law requires labels to list the eight major food allergens: milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soy. If you’re allergic, that’s your first safety net. But that’s it. No warnings about interactions with blood thinners, thyroid meds, diabetes drugs, or antidepressants. Not even a hint.
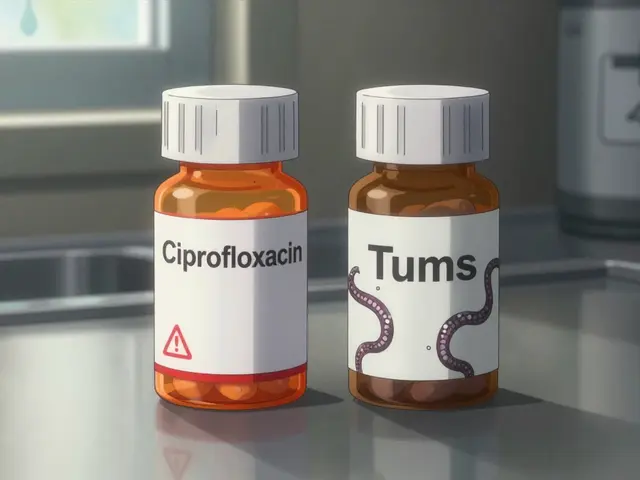
Compare that to a bottle of ibuprofen. It has a full Drug Facts panel. It tells you exactly what’s in it, what it’s for, how to take it, and-crucially-what other drugs it shouldn’t be mixed with. That’s because the FDA requires it. Supplements? No such rule.
Why Drug Labels Are So Much Clearer
Prescription and OTC drug labels are tightly controlled. The FDA demands that every possible interaction be studied and listed. About 97% of prescription drugs include interaction warnings. OTC meds? Around 90%. But for supplements? Only about 13% do.
Take warfarin, a common blood thinner. If you take vitamin K supplements-like green tea extract or certain multivitamins-your blood won’t clot properly. Studies show vitamin K can cut warfarin’s effectiveness by up to 50%. But you won’t see that on the supplement bottle. You’ll only find it if you look up the ingredients yourself.
St. John’s wort is another silent danger. It’s sold as a natural mood booster. But it can drop digoxin levels by 26%. That’s enough to cause heart failure in someone relying on that drug. CoQ10? It can shorten prothrombin time by 15-25%, again raising clotting risks for people on blood thinners. And vitamin C? Doses over 1,000 mg a day can reduce the effectiveness of some HIV meds by 22%.
None of these warnings are required on supplement labels. The FDA doesn’t force manufacturers to test for them. So they don’t. And consumers? They assume the label is complete. It’s not.
The Hidden Dangers of Proprietary Blends
Proprietary blends are the biggest trap. They let companies hide ingredient amounts. One popular pre-workout supplement had 1,200 mg of a blend labeled “Energy Matrix.” Inside? Caffeine, yohimbine, and green tea extract. But how much of each? No idea. One study found 38% of supplements use blends to conceal how much of a potent ingredient they’re really giving you.
Red yeast rice is another example. It’s sold as a “natural” cholesterol reducer. But it contains monacolin K-the exact same compound as the prescription drug lovastatin. If you’re already on a statin, taking this supplement can cause muscle damage or kidney failure. But the label doesn’t say that. It just says “red yeast rice.”
And don’t be fooled by words like “natural,” “herbal,” or “pure.” Those mean nothing in terms of safety. They’re marketing terms, not safety guarantees.
How to Protect Yourself: A Simple 5-Step Plan
You don’t need a pharmacy degree to stay safe. Just follow these steps:
- Write down every supplement you take. Include brand, dose, and frequency. Don’t rely on memory.
- Take a photo of the label. Keep it on your phone. Show it to your doctor or pharmacist every time you visit.
- Check each ingredient against a trusted database. Use the free Medscape Drug Interaction Checker. It analyzes over 24,000 drug and supplement pairs. Type in your med and the supplement name. If it says “major interaction,” stop taking it.
- Ask your pharmacist. Pharmacists are trained to spot interactions. They see hundreds of drug-supplement combos a week. Don’t be shy. Say: “I’m taking this supplement with my blood pressure med. Is that safe?”
- When in doubt, pause. If you’re unsure, don’t take it. Wait until you’ve talked to a professional. It’s better to delay a supplement than risk a hospital visit.
Real People, Real Consequences
People are getting hurt. On Reddit’s r/Supplements forum, over 1,800 people have shared stories of confusion. One user took magnesium with levothyroxine for thyroid issues. The label said nothing. He didn’t know magnesium blocks absorption. His TSH levels shot up. He ended up with fatigue, weight gain, and depression-all because he trusted the label.
A woman with type 2 diabetes added milk thistle to her routine to “support her liver.” It lowered her blood sugar too much. She collapsed at home. Her glucose dropped to 42 mg/dL. She survived, but barely. She didn’t know milk thistle can amplify metformin’s effects.
A 2023 survey found 47% of supplement users keep taking them even while on prescription drugs-because the labels don’t warn them. That’s not ignorance. That’s a system failure.
What’s Being Done? (And Why It’s Not Enough)
The supplement industry is worth $53 billion. Yet the FDA’s entire office dedicated to supplements has a budget of $4.7 million-less than 0.03% of the FDA’s total spending. In 2023, they found over 1,200 supplements with false or dangerous labels. Only 28% of those led to recalls.
There’s hope, though. In March 2024, the FDA released draft guidance suggesting supplement labels voluntarily include interaction warnings. But voluntary means most won’t do it. The American Medical Association now recommends doctors spend 3-5 minutes during yearly checkups asking patients about supplements. That’s a start.
Some brands are stepping up. Less than 20% carry the USP Verified mark. That means an independent lab tested the product for purity, potency, and label accuracy. If you see USP on the bottle, you’re getting something more reliable. But most don’t have it.
Future changes might include QR codes on labels that link to real-time interaction data. But until laws change, you’re still the last line of defense.
Bottom Line: You’re the Safety Net
The system isn’t built to protect you. It’s built to let supplements be sold fast and cheap. That’s the reality. The FDA doesn’t approve supplements before they hit shelves. They don’t test them for interactions. They don’t even require warnings.
So you have to do the work. Don’t assume. Don’t guess. Don’t trust the word “natural.” Write it down. Photograph it. Check it. Ask your pharmacist. If your doctor doesn’t ask about your supplements, bring it up. Most don’t know enough to ask.
Supplements aren’t harmless. They’re powerful. And like any medicine, they can hurt you if used carelessly. The label doesn’t tell you the truth? Then find the truth yourself. Your life might depend on it.
Do supplement labels have to list drug interactions?
No. Unlike prescription and over-the-counter drugs, supplement manufacturers are not required by law to list drug interactions on their labels. The FDA does not mandate interaction warnings for dietary supplements under the Dietary Supplement Health and Education Act (DSHEA) of 1994. Only about 13% of supplement products voluntarily include such warnings, according to FDA data.
What should I do if my supplement doesn’t warn about interactions?
Don’t assume it’s safe. Use the Medscape Drug Interaction Checker or consult your pharmacist with the supplement’s ingredient list. Take a photo of the label and show it to your doctor during your next visit. If you’re on blood thinners, thyroid meds, diabetes drugs, or antidepressants, even a seemingly harmless supplement like vitamin K, St. John’s wort, or magnesium can cause serious problems.
Are ‘natural’ supplements safer than prescription drugs?
No. ‘Natural’ doesn’t mean safe. Red yeast rice contains the same active ingredient as the prescription statin lovastatin. St. John’s wort can reduce blood levels of digoxin by 26%, leading to heart complications. Green tea extract can interfere with warfarin. Many natural substances are potent and can interact dangerously with medications. Always treat supplements like medicine.
What’s a proprietary blend, and why is it dangerous?
A proprietary blend lists multiple ingredients together without showing how much of each is in the product. This lets manufacturers hide high doses of potent substances. For example, a pre-workout might say ‘Energy Matrix: 1,200 mg’-but you won’t know if it’s mostly caffeine or a tiny bit of yohimbine. That makes it impossible to assess safety or interaction risk. About 38% of supplements use this trick, according to ConsumerLab.com.
Can I trust supplements with the USP Verified mark?
Yes. The USP Verified mark means an independent lab tested the product for accurate ingredient amounts, purity, and proper manufacturing. USP-certified supplements have 92% label accuracy, compared to just 67% for non-certified ones. While it doesn’t guarantee interaction safety, it ensures you’re getting what the label says you’re getting-something most supplements can’t promise.
Should I stop taking supplements before surgery?
Yes. Many supplements-like fish oil, garlic, ginkgo, and vitamin E-can increase bleeding risk during surgery. Others, like St. John’s wort or kava, can interfere with anesthesia. Most surgeons recommend stopping all supplements at least 1-2 weeks before any procedure. Always tell your surgical team exactly what you take, even if it’s ‘just a vitamin.’





Reviews