Finding a lump on your adrenal gland by accident can be terrifying. You didn’t have symptoms. You weren’t even looking for anything. Then a CT scan or MRI for back pain, a car accident, or a routine checkup shows a small mass - and suddenly, you’re drowning in medical terms: adrenal incidentaloma, functional tumor, malignancy risk, dexamethasone test. What does it all mean? And more importantly - do you need surgery?
What Exactly Is an Adrenal Incidentaloma?
An adrenal incidentaloma is simply a tumor on one or both adrenal glands that shows up by chance during imaging done for another reason. It’s not something you felt, didn’t cause symptoms, and wasn’t suspected. These masses are surprisingly common - about 2% of adults have one. By age 70, that number jumps to over 7%. With more people getting CT scans these days, we’re finding them more often than ever.
The adrenal glands sit on top of your kidneys. They make hormones that control blood pressure, metabolism, stress response, and sex drive. Most adrenal tumors are harmless - about 80% are benign, non-functioning adenomas. They just sit there. But 20% can be dangerous: either they make too much hormone (functional) or they’re cancerous (malignant). That’s why every incidentaloma needs evaluation - even if you feel fine.
The Three Types of Adrenal Tumors You Might Have
Not all adrenal masses are the same. They fall into three clear groups:
- Functioning tumors: These make extra hormones. The most common are cortisol-producing (causing subclinical Cushing’s), aldosterone-producing (raising blood pressure), and pheochromocytomas (making adrenaline spikes). These can cause serious problems even without obvious symptoms.
- Malignant tumors: These include primary adrenocortical carcinoma (rare but aggressive) or cancer that spread to the adrenal gland from elsewhere, like lung or breast cancer.
- Benign non-functioning tumors: These are the most common - about 80%. They include adenomas, myelolipomas (fat-filled tumors), cysts, and hematomas. They don’t make hormones and rarely grow. Often, they’re just watched - or ignored.
Knowing which type you have changes everything. A pheochromocytoma needs urgent treatment. A small, stable adenoma might not need any.
Step-by-Step Evaluation: What Tests You’ll Actually Get
There’s a clear, evidence-based path for evaluating these tumors. It’s not guesswork. Here’s what happens in real clinical practice:
- Unenhanced CT scan: This is the first test. If the tumor has a density below 10 Hounsfield units, it’s likely a benign adenoma - about 70-80% chance. No further imaging is needed unless it’s large or looks weird.
- Test for pheochromocytoma: This is non-negotiable. Every single adrenal mass must be checked for excess adrenaline. You’ll get either a 24-hour urine test for metanephrines or a blood test for plasma-free metanephrines. If this is missed and you have surgery without treatment, you could have a deadly blood pressure spike during anesthesia.
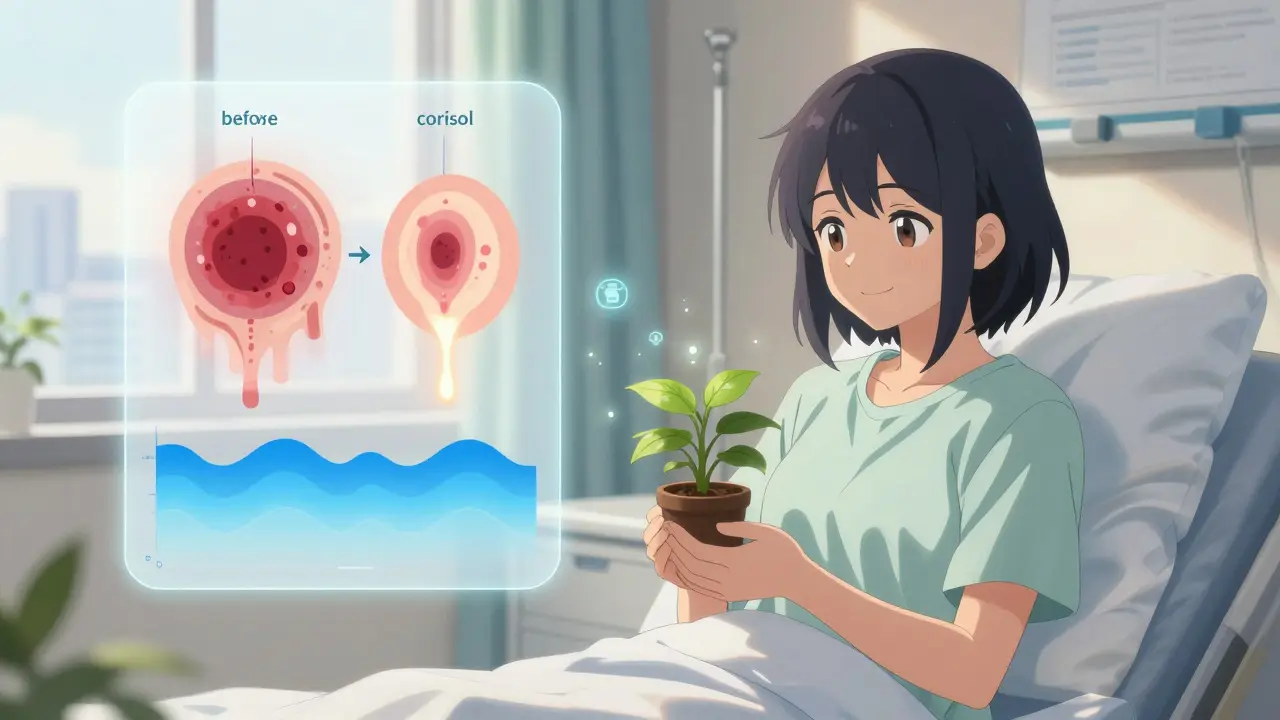
- Test for cortisol excess: You’ll get a 1-mg dexamethasone suppression test. If your cortisol level stays above 1.8 μg/dL after the pill, you may have autonomous cortisol secretion - also called subclinical Cushing’s. This affects about 5% of incidentalomas and increases your risk of diabetes, heart disease, and bone loss, even if you don’t look like you have Cushing’s.
- Test for aldosterone: Only if you have high blood pressure or low potassium. You’ll check plasma aldosterone and renin. If aldosterone is high and renin is low, you likely have an aldosterone-producing adenoma - which can be cured with surgery.
These tests are simple, non-invasive, and widely available - but not always ordered. Many community hospitals don’t have quick access to metanephrine testing. That’s a problem. If your doctor doesn’t order these, ask why.

When Is Surgery Actually Needed?
Surgery isn’t automatic. It’s reserved for specific, high-risk cases. Here’s the hard line:
- All functional tumors: Whether it’s making cortisol, aldosterone, or adrenaline - surgery is recommended. These cause real, measurable harm over time. Removing the tumor often reverses high blood pressure, diabetes, or heart rhythm problems.
- Tumors larger than 4 cm: Size matters. Tumors under 4 cm have less than a 1% chance of being cancer. Between 4 and 6 cm, the risk jumps to 5-10%. Above 6 cm? The chance of adrenocortical carcinoma is 25%. That’s not a gamble you take.
- Suspicious imaging features: If the tumor looks irregular, has uneven texture, or grows fast (more than 1 cm per year), it’s flagged for surgery - even if it’s under 4 cm.
- Confirmed cancer or metastasis: If it’s clearly malignant, surgery is the first step - if you’re healthy enough for it.
For small, non-functioning tumors under 4 cm with normal imaging? No surgery. No follow-up scans. Just move on. Many patients are told to come back every year for scans - that’s outdated. The Endocrine Society says routine follow-up isn’t needed unless something looks off.
The Hidden Danger: Subclinical Cushing’s Syndrome
This is the trickiest part. You might not look sick. No moon face, no purple stretch marks. But your body is still flooded with too much cortisol. That’s subclinical Cushing’s - and it’s more common than you think. Studies show it affects 5-10% of adrenal incidentalomas.
Here’s what it does quietly: raises blood sugar, increases belly fat, weakens bones, raises blood pressure, and increases heart attack risk. A 2023 study showed that patients with cortisol levels above 5.0 μg/dL after dexamethasone had clear metabolic improvements after surgery. That’s why the Endocrine Society is updating its guidelines to be more aggressive about treating these cases.
Doctors still debate the best test. The dexamethasone suppression test isn’t perfect. But a new test - urinary steroid metabolomics - is showing 92% accuracy. It’s not everywhere yet, but it’s coming.
What Happens Before Surgery?
If you’re scheduled for removal, preparation is critical - especially for pheochromocytoma. You can’t just go under anesthesia. You need alpha-blockers (like phenoxybenzamine) for at least 7 to 14 days before surgery. This controls your blood pressure and prevents a surge during the operation. Skip this step, and you could die on the table.
For cortisol-secreting tumors, doctors may give you hydrocortisone before and after surgery to help your body adjust. Your adrenal gland has been making too much hormone - suddenly stopping it can crash your system.
Most adrenal surgeries today are done laparoscopically. Small cuts, fast recovery. Most people go home in 1-2 days.
Why You Should Go to a Specialized Center
This isn’t a routine procedure for most hospitals. Only 37 U.S. hospitals are designated as Comprehensive Adrenal Centers. At these places, endocrinologists, radiologists, and surgeons work together daily. They’ve seen hundreds of cases. They know which scans to trust. They order the right tests. They avoid unnecessary surgeries.
One 2023 survey found 92% of patients treated at specialized centers were satisfied with their care. At general hospitals? Only 68%. The difference isn’t just skill - it’s coordination. A misread CT scan or missed metanephrine test can lead to wrong decisions. And those decisions last a lifetime.
What About Tiny Tumors - Under 1 cm?
Some guidelines say anything under 1 cm doesn’t count as an incidentaloma. Others - like the European Society - still evaluate anything over 1 cm. The truth? Tumors under 1 cm are almost always benign. Most experts agree they don’t need testing unless they’re growing or you have symptoms. But if you’re anxious and your doctor finds one, it’s reasonable to get a basic hormone check. Just don’t get swept into endless scans.
The Big Picture: Why This Matters
Over 4 million adrenal incidentalomas are found in the U.S. every year. That’s a lot of scans, tests, and stress. The cost? Around $1.2 billion annually. But the real cost is the anxiety patients feel. One informal survey of 142 patients found 78% were deeply stressed waiting for results.
But here’s the good news: if you’re evaluated properly, most of these tumors are harmless. And if you have something dangerous, catching it early saves your life. The key is following the science - not fear.
Don’t let a random scan send you down a rabbit hole. Get the right tests. Ask if your doctor is following the Endocrine Society guidelines. If they’re not, ask why. And if surgery is recommended, make sure you’re being treated by a team that does this regularly.
You didn’t ask for this. But now that you have it, you deserve a clear, evidence-based path forward - not confusion, not delays, not guesswork.
Do all adrenal incidentalomas need surgery?
No. About 80% of adrenal incidentalomas are benign, non-functioning tumors that don’t require any treatment. Surgery is only recommended for tumors larger than 4 cm, those that produce excess hormones, or those with imaging features suggesting cancer. Most small, stable tumors can be safely ignored.
Can an adrenal incidentaloma cause symptoms?
By definition, an incidentaloma is found without symptoms. But if it’s functional - meaning it makes too much hormone - it can cause problems later. Cortisol excess can lead to weight gain, high blood pressure, or diabetes. Aldosterone can raise blood pressure. Pheochromocytomas can cause sudden spikes in heart rate and blood pressure. So while you may feel fine now, untreated functional tumors can harm you over time.
What’s the biggest risk of not evaluating an adrenal incidentaloma?
The biggest risk is missing a pheochromocytoma. If this tumor isn’t detected before surgery, the stress of anesthesia can trigger a massive adrenaline surge, causing a fatal spike in blood pressure. That’s why testing for metanephrines is mandatory for every adrenal mass - no exceptions.
How accurate is a CT scan in telling if an adrenal tumor is cancerous?
CT scans are very good at identifying benign adenomas - especially if the density is under 10 Hounsfield units. But they’re less reliable for spotting early cancers. A tumor that looks smooth and uniform might still be malignant. Size and growth rate matter more. Tumors over 4 cm, with irregular edges, or growing fast are more likely to be cancerous, even if the CT looks normal.
Should I get a second opinion if my doctor says I need surgery?
Yes - especially if it’s a large tumor or you’re being told to have surgery without full hormonal testing. Adrenal surgery is complex and should be done by teams experienced in endocrine surgery. Ask if your doctor is following the Endocrine Society guidelines. If you’re unsure, seek care at a specialized adrenal center. They’ll review your scans, confirm your hormone tests, and help you understand if surgery is truly necessary.
Is there a blood test that can confirm if a tumor is making too much cortisol?
The standard test is the 1-mg dexamethasone suppression test. If your cortisol stays above 1.8 μg/dL after taking the pill, it suggests autonomous secretion. A newer test - urinary steroid metabolomics - is more accurate and detects cortisol excess in 92% of cases. It’s not widely available yet, but it’s becoming the new gold standard.
How long does recovery take after adrenal surgery?
Most adrenal surgeries today are done laparoscopically. Patients usually go home within 1-2 days. Full recovery takes about 2-4 weeks. If you had a cortisol-secreting tumor, you may need to take steroid replacement for a few months while your other adrenal gland wakes up. Your doctor will monitor your hormone levels closely during this time.
Can adrenal incidentalomas come back after surgery?
If you had a benign adenoma removed, it won’t come back. But if you had cancer - especially adrenocortical carcinoma - there’s a risk of recurrence. That’s why long-term follow-up is needed in those cases. For functional tumors like pheochromocytoma or aldosterone-producing adenomas, recurrence is rare after complete removal. Most patients see full resolution of symptoms like high blood pressure or diabetes.





Reviews