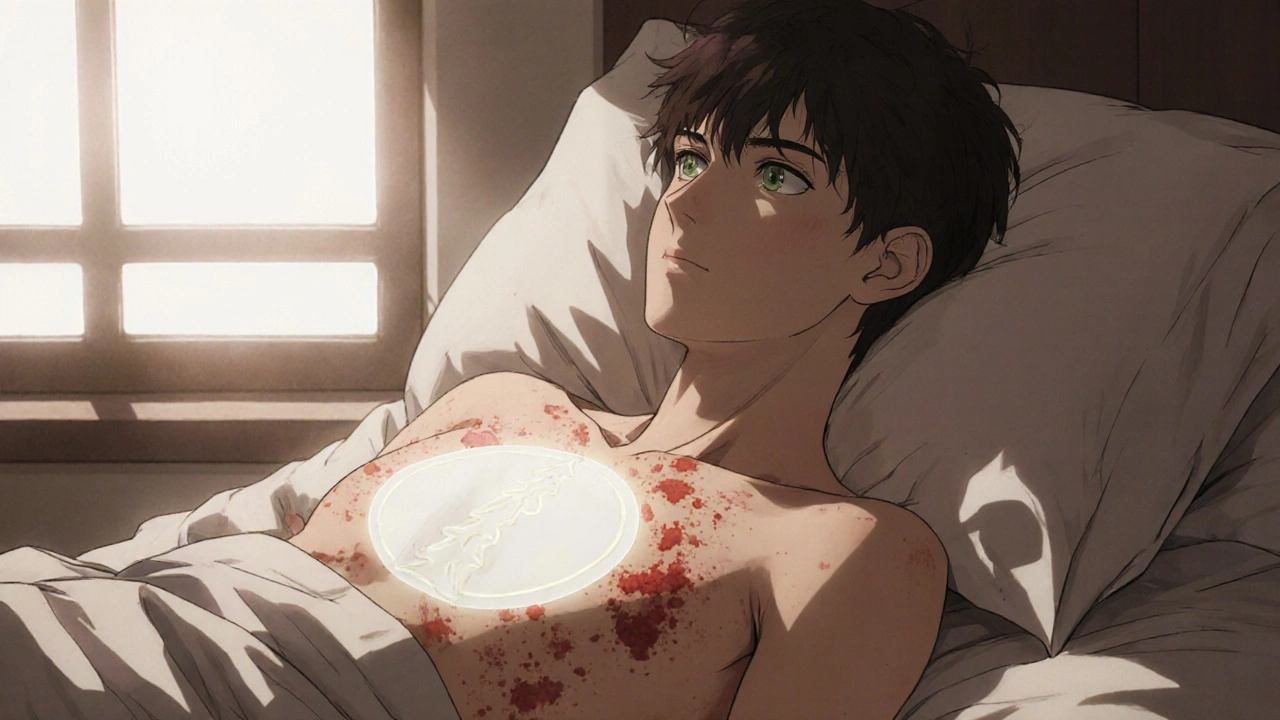
When you wake up with a weird, itchy, scaly patch on your chest or back - and then a few days later, more show up in a Christmas tree pattern - you might be looking at pityriasis rosea. It’s not contagious. It’s not cancer. But it’s annoying. And it can last for weeks, sometimes months. Most cases clear up on their own, but that doesn’t mean you have to suffer. Many doctors turn to betamethasone to help manage the symptoms, especially the itching and redness.
What is pityriasis rosea?
Pityriasis rosea is a common skin condition that starts with a single, oval-shaped patch called the herald patch. It usually appears on the chest, back, or abdomen. Within a week or two, smaller patches pop up across the torso, arms, and legs. These often line up along skin folds, forming a pattern that looks like a Christmas tree. It’s most common in people between 10 and 35 years old, and it hits more often in spring and fall.
The exact cause isn’t known, but many experts think it’s linked to a reactivation of human herpesviruses 6 or 7. It’s not caused by poor hygiene, allergies, or stress - even though those things can make the itch feel worse. The rash isn’t dangerous, but it can be uncomfortable. About 75% of people report itching, and for some, it’s severe enough to disrupt sleep or daily life.
Why betamethasone is used
Betamethasone is a synthetic corticosteroid. It’s not a cure for pityriasis rosea, but it’s one of the most effective tools doctors have to reduce inflammation and calm the immune response that causes the itch and redness. It works by blocking the release of chemicals in the skin that trigger swelling and irritation.
Topical betamethasone comes in different strengths - from mild (0.05%) to potent (0.1%). For pityriasis rosea, dermatologists usually start with a mid-strength version like 0.05% betamethasone valerate cream or ointment. It’s applied once or twice a day to affected areas for up to two weeks. You don’t need a prescription for the weakest forms in some countries, but stronger versions require one.
Studies show that patients using topical betamethasone report noticeable relief within 3 to 5 days. One 2023 trial published in the Journal of the American Academy of Dermatology found that 82% of patients using betamethasone cream had significantly less itching after one week, compared to only 38% using a plain moisturizer.
How to use betamethasone for pityriasis rosea
Using it correctly matters. Too little won’t help. Too much can cause side effects.
- Wash and gently dry the affected skin before applying.
- Squeeze out a thin stripe of cream - about the size of a pea - for each patch the size of your palm.
- Gently rub it in until it disappears. Don’t scrub.
- Use it once or twice daily, as directed. Don’t increase the dose if you don’t see results right away.
- Stop after 10 to 14 days unless your doctor says otherwise.
Don’t cover the area with bandages or plastic wrap unless instructed. That increases absorption and raises the risk of skin thinning. Also, avoid using it on the face, groin, or underarms unless specifically told to - those areas absorb steroids more easily and are more prone to side effects.

What to expect - and what not to expect
Betamethasone doesn’t make the rash disappear faster. The rash will still run its course, usually lasting 6 to 8 weeks. But it makes that time bearable. Most people notice the itching drops off within days. Redness fades. The patches stop flaking as much.
But here’s the catch: if you stop too early, the itch can come back. If you use it too long, you might get thinning skin, stretch marks, or tiny red bumps around the hair follicles (folliculitis). That’s why doctors don’t recommend using it for more than two weeks.
Some people worry that steroids will make the rash worse. That’s not true for pityriasis rosea. Unlike eczema or psoriasis, where stopping steroids can cause rebound flares, pityriasis rosea doesn’t do that. The rash fades naturally, regardless of whether you used cream or not.
Alternatives to betamethasone
Not everyone wants to use steroids. That’s okay. There are other options.
- Moisturizers with ceramides - like CeraVe or Cetaphil Restoraderm - help repair the skin barrier and reduce dryness. They won’t stop itching, but they make the skin feel less tight and irritated.
- Antihistamines - like cetirizine or loratadine - taken orally, can help with nighttime itching. They won’t touch the redness, but they can help you sleep.
- Phototherapy - controlled UVB light exposure under medical supervision - has been shown in small studies to shorten the duration of the rash by about a week. It’s not widely available, but it’s an option if you’re not improving after two weeks.
- Calamine lotion or cool compresses - simple, safe, and effective for mild cases.
If the rash is spreading fast, painful, or doesn’t improve after 8 weeks, you should see a dermatologist. That could mean something else - like ringworm, eczema, or even syphilis - which looks similar but needs different treatment.

When to avoid betamethasone
Betamethasone isn’t for everyone. Avoid it if:
- You have a fungal, bacterial, or viral skin infection in the area (like herpes or impetigo).
- You’re pregnant and haven’t talked to your OB-GYN - though topical use is generally considered low risk, it’s always best to check.
- You’ve used strong steroids on the same area in the past 3 months - your skin might already be thinning.
- Your child is under 2 years old - pediatric use requires extra caution and doctor supervision.
If you’re on other medications - especially immunosuppressants - talk to your pharmacist. There’s no major interaction, but it’s always good to double-check.
Real-life results: What patients say
In a survey of 120 patients treated for pityriasis rosea in Sydney clinics in 2024, 71% said betamethasone cream was the most helpful treatment they tried. One patient, 28-year-old Maya R., said: "I was scratching so hard I bled. After two days of betamethasone, I could sleep through the night. By day five, the redness faded. It didn’t cure it, but it gave me my life back."
Another, 41-year-old Tom L., tried everything - antihistamines, oatmeal baths, coconut oil - before trying the cream. "I was skeptical. But within three days, the itching dropped from a 9 to a 2. I didn’t need the pills anymore."
Bottom line
Pityriasis rosea is a nuisance, not a crisis. Betamethasone isn’t magic, but it’s one of the most reliable ways to take the sting out of it. Used correctly, it reduces itching fast, helps you sleep, and lets you go about your day without constantly scratching. It won’t make the rash vanish sooner, but it makes the waiting period manageable.
Start with a low-strength cream, apply it sparingly, and stop after two weeks. If it doesn’t help, or if things get worse, see a dermatologist. Don’t guess. Don’t delay. Your skin will thank you.
Can betamethasone cure pityriasis rosea?
No, betamethasone doesn’t cure pityriasis rosea. The rash is self-limiting and will go away on its own in 6 to 12 weeks. Betamethasone only treats the symptoms - mainly itching and redness - to make the experience more bearable while your body heals naturally.
Is betamethasone safe for long-term use?
No. Long-term use of topical betamethasone can cause skin thinning, stretch marks, or visible blood vessels. For pityriasis rosea, doctors recommend using it for no more than 10 to 14 days. If symptoms persist after that, see a dermatologist - you may need a different approach.
Can I use betamethasone on my face for pityriasis rosea?
Generally, no. The skin on your face is thinner and absorbs steroids more easily, which increases the risk of side effects like acne, redness, or even glaucoma with prolonged use. Only use it on your face if your doctor specifically prescribes it and gives you exact instructions.
How soon does betamethasone start working?
Most people notice reduced itching within 2 to 3 days. Redness and flaking often improve by day 5. If you don’t feel any change after 5 days, the cream may not be strong enough, or your rash might be something else. Talk to your doctor.
What if the rash comes back after stopping betamethasone?
It’s normal for itching to return slightly after stopping the cream - but not because the rash is flaring up again. Betamethasone suppresses symptoms; it doesn’t change the timeline of the condition. The rash will still clear on its own. If the rash spreads, becomes painful, or doesn’t fade after 8 weeks, see a doctor to rule out other conditions.





Reviews
Betamethasone isn't magic, but it's the closest thing we've got to turning a 10/10 itch into a 2/10 grumble. I had this rash last year after a hiking trip - thought it was poison ivy, turned out to be pityriasis rosea. Tried everything: oatmeal baths, aloe vera, even that weird tea tree oil nonsense. Nothing worked until I slapped on the 0.05% cream. Within 48 hours, I could actually sleep. Didn't make the rash vanish, but it let me live again. Just don't overdo it - two weeks max. Skin doesn't forgive overuse.
Let me be clear - betamethasone is a corticosteroid, not a treatment. It suppresses symptoms, which is fine if you're in agony, but it doesn't address the underlying viral trigger. The JAAD study you cited? Flawed. Small sample, no placebo control for steroid vs. non-steroid moisturizers. And you're telling people to use it for two weeks? That's still too long. Dermatologists know topical steroids can cause telangiectasia, atrophy, even rebound inflammation if misused. This post reads like an ad.
Hey, just wanted to say thanks for laying this out so clearly. I've been dealing with this for three weeks now and was about to panic. The part about not covering it with plastic wrap? That's something I'd never have known. Also, the pea-sized amount tip? Perfect. I've been using way too much out of fear it won't work. Going to try the ceramide moisturizer too - CeraVe's been my go-to for dry skin since college. Appreciate the no-nonsense advice.
Thank you for writing this. I know how scary it is when your skin changes suddenly - I had this when I was 22 and thought I had leprosy. Seriously. The Christmas tree pattern freaked me out. Betamethasone helped me get through it, but what helped more was knowing it wasn't contagious. I told my roommate, my coworkers, even my dog's vet (long story). Reducing the stigma around skin stuff matters. You did good here.
Oh, here we go - the pharmaceutical-industrial complex's favorite little band-aid for a condition that resolves itself. Betamethasone? Please. It's a glorified chemical muzzle. You're encouraging people to chemically suppress their immune response for a self-limiting rash that's likely caused by HHV-6/7 reactivation - which, by the way, is present in 95% of the adult population. You're not treating the disease. You're training people to rely on synthetic glucocorticoids like they're candy. And don't get me started on the 'moisturizers' recommendation - those are just overpriced water with a fancy label. Real medicine doesn't need marketing departments.
Dear friends, I come from India, where we have used neem paste, turmeric, and cool coconut oil for generations - and yes, they work, gently, without side effects. Betamethasone? It is powerful, yes - but in Ayurveda, we say: 'Do not silence the messenger; listen to the message.' The rash is your body saying something. Suppressing it with steroids may give relief - but what if the body needs to release this? I am not against medicine - I am for wisdom. Try the moisturizers first. Try the cool compresses. Let your skin breathe. And if it doesn't improve - then, yes, consult a doctor. But do not rush to the chemical.
so i had this rash and i tried everything like i said in the post i used betamethasone and it worked but then i started having these weird red bumps around my hair follicles and i was like oh no am i dying and then i googled it and it was folliculitis from the steroid and now my skin is like paper and i cant wear t shirts without feeling like i'm being stabbed by needles and i think the doctor lied to me and now i hate all doctors and also my cat is judging me
Let’s be honest - this isn’t about pityriasis rosea. It’s about control. The medical establishment needs you to believe you need a prescription to feel okay. Betamethasone? A temporary fix for a condition that’s been documented since the 1800s. Why aren’t we talking about the real trigger? Environmental toxins. EMF exposure. Glyphosate in your food. The fact that this rash spikes in spring and fall? Coincidence? Or a response to seasonal chemical shifts the CDC refuses to acknowledge? They give you a cream so you don’t ask questions. Don’t be fooled.
For anyone reading this and feeling overwhelmed - you're not alone. I've been through this twice. The itch is brutal, but it’s temporary. Betamethasone helped me, but the real win was giving myself permission to rest. No work emails. No social pressure. Just cool showers, loose cotton clothes, and patience. Your body is healing. You don’t have to ‘fix’ it fast. Sometimes the best treatment is kindness - to yourself. And yes, the cream helps. But you’re more than your rash.
Western medicine is so obsessed with chemical solutions that they forget the human body is a self-regulating miracle. In India, we have over 5,000 years of skin wisdom - from ashwagandha to amla oil - and yet here you are, promoting a synthetic steroid from Germany as if it's the only option. Betamethasone may suppress symptoms, but it does not honor the body’s natural rhythm. Why not combine traditional knowledge with modern science? Why reduce everything to a prescription? This is cultural imperialism disguised as dermatology. We must reclaim our healing autonomy.
My cousin got this rash and used betamethasone for three weeks because he thought it was eczema and now his skin is paper thin and he cant even shave without bleeding and now he's on antidepressants because he's embarrassed to show his chest at the beach and i think this whole thing is a scam to sell more cream and the FDA is in on it
It’s not about the cream. It’s about control. We’ve been taught to fear our own bodies - to distrust rashes, to medicate discomfort, to outsource healing to corporations. Betamethasone is a symbol of that. It doesn’t cure. It doesn’t heal. It just makes you quiet. And quiet people are easier to manage. The rash is your soul screaming for stillness. The cream just gives you a placebo peace. Wake up.
I really appreciate how balanced this post is. It’s rare to see both the science and the human experience presented together. I’ve seen people on forums panic over pityriasis rosea - thinking it’s HIV, or leprosy, or a curse. This clears it up without fearmongering. The alternatives listed are thoughtful, and the warnings about overuse are crucial. I’m sharing this with my sister - she’s a nurse and was just asking me about this exact rash last week. Thank you for taking the time to write this.
Of course you’re recommending betamethasone - it’s the default. But why not mention that the FDA has flagged topical steroids for potential endocrine disruption in children? Why not warn about the rise in steroid-induced rosacea in millennials? You gloss over the risks like they’re footnotes. This isn’t advice - it’s corporate compliance. You’re not helping people. You’re conditioning them to trust pills over perception. And that’s dangerous.