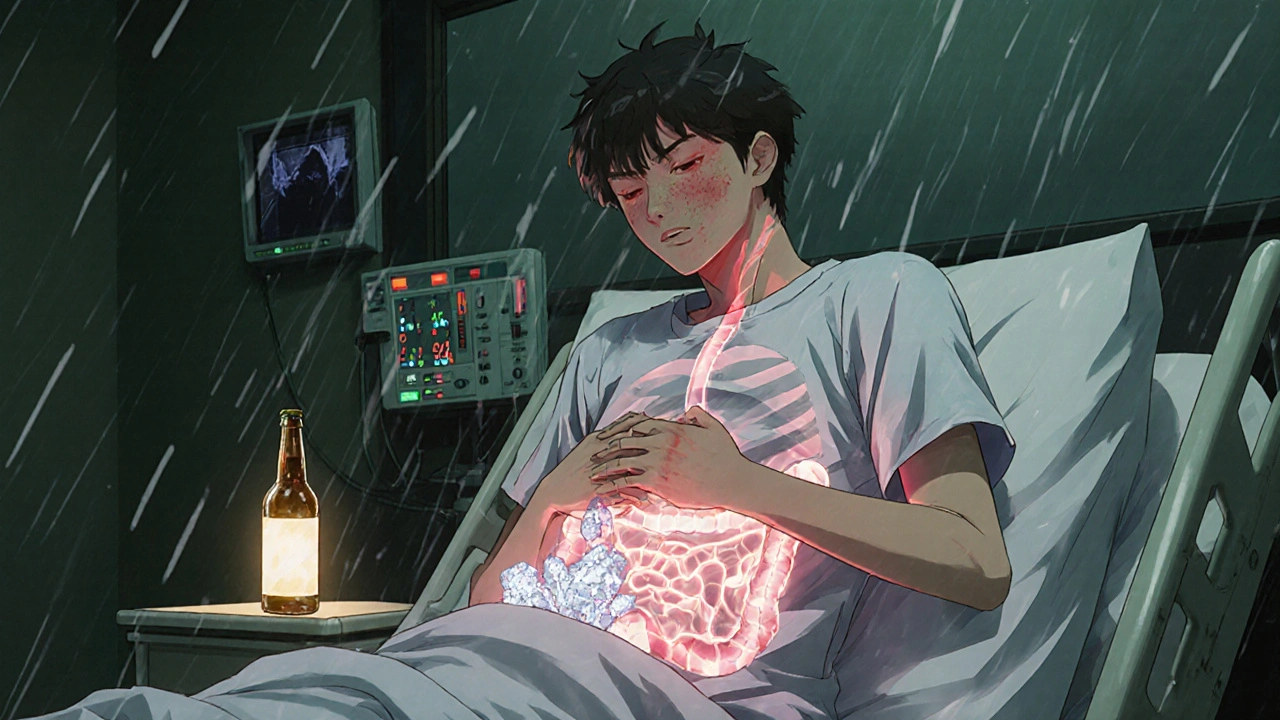
When you’re dealing with stomach bugs, diarrhea, or acid reflux, you reach for your meds. But if you’ve had a drink or two, you might not realize how much alcohol is messing with what your body’s trying to fix. It’s not just about feeling dizzy or nauseous. Alcohol doesn’t just add to the side effects of digestive meds-it can change how they work, make them useless, or even turn them dangerous.
Alcohol Slows Down Your Digestion-And Your Meds
Alcohol doesn’t just sit in your stomach. It gets absorbed fast, especially on an empty stomach, and hits your liver before your meds even finish being processed. Your liver is the main factory that breaks down both alcohol and most digestive medications. When you mix them, your liver gets overloaded. It starts prioritizing alcohol because it’s a toxin. That means your meds-like loperamide, ranitidine, or omeprazole-don’t get broken down the way they should. They either stick around too long or don’t work at all.
Take loperamide (Imodium). It’s meant to slow your gut so diarrhea stops. Alcohol does the same thing. When you mix them, your bowels can slow down too much. That’s not just uncomfortable-it can lead to dangerous constipation, bloating, or even bowel obstruction. And if you’re already dehydrated from a stomach bug, alcohol makes it worse. You’re not just fighting the bug anymore. You’re fighting your own meds.
There’s a real case from a Bristol GP last year: a 42-year-old man took his usual dose of loperamide after a night out. He didn’t think twice-after all, he’d had a beer with it before. But this time, he ended up in A&E with severe abdominal pain and no bowel movement for 72 hours. His blood tests showed loperamide levels three times higher than normal. The alcohol had blocked his liver from clearing the drug. He needed a hospital stay and a laxative drip. You can read more about the risks of combining loperamide and alcohol can you drink alcohol with Imodium.
Acid Reflux Meds? Alcohol Makes It Worse
If you’re on omeprazole or famotidine for heartburn, you might think alcohol is just a minor issue. It’s not. Alcohol relaxes the lower esophageal sphincter-the muscle that keeps stomach acid from creeping up. That’s why you get that burning feeling after wine or whiskey. But when you take acid-reducing meds, your body expects the acid to stay down. Alcohol overrides that. It doesn’t matter if you took your pill an hour ago. Alcohol still triggers acid production and weakens the barrier. You end up with worse reflux than before you took the med.
And here’s the kicker: long-term alcohol use can actually make your stomach produce more acid over time. That means your meds become less effective. You might start doubling your dose, thinking it’s not working. But it’s not the med. It’s the alcohol.
Antibiotics and Gut Meds Don’t Play Nice
Antibiotics like amoxicillin or metronidazole are common for gut infections. But mixing them with alcohol? Bad idea. Metronidazole, in particular, can cause a nasty reaction: flushing, vomiting, rapid heartbeat, and even chest pain. It’s called a disulfiram-like reaction. Your body can’t break down the alcohol properly when metronidazole is in your system. The result? You feel like you’re having a heart attack.
Even if your antibiotic doesn’t have that reaction, alcohol still messes with your gut flora. Antibiotics kill bad bacteria-but they also kill the good ones. Alcohol does the same thing. Together, they wipe out your microbiome. That’s why people often get worse diarrhea after antibiotics-even when they’re taking probiotics. Alcohol just adds fuel to the fire.
Why Some People Think It’s Fine
You’ve probably heard: “I had a glass of wine with my pill and nothing happened.” That’s true-for some people. But that doesn’t mean it’s safe. Everyone’s liver works differently. Age, weight, genetics, and how often you drink all change how your body handles the mix. Someone in their 20s might get away with it. Someone over 50? Not a chance. Your liver slows down as you age. Alcohol sticks around longer. So does your med.
Also, many people don’t realize that even “non-alcoholic” beer has up to 0.5% alcohol. That’s enough to interfere with meds if you’re drinking more than one. Same with mouthwash, cough syrups, and some supplements. They’re not just water.
What to Do Instead
If you’re on digestive meds, treat alcohol like a wildcard. Don’t assume it’s harmless. Here’s what actually works:
- Wait 4-6 hours after your last dose before having a drink. That gives your body time to clear the med.
- Never drink on an empty stomach. Food slows alcohol absorption. Even a slice of toast helps.
- Stick to one drink, max. If you’re on daily meds like omeprazole, skip it entirely. One drink isn’t worth the risk.
- Hydrate like crazy. Drink water before, during, and after. Alcohol dehydrates. Your gut needs fluids to heal.
- Track your symptoms. If you feel bloated, dizzy, or your diarrhea gets worse after drinking, stop. It’s not normal.

When to Call Your Doctor
Some reactions are obvious. Others sneak up on you. Call your doctor if you notice:
- Severe constipation (no bowel movement for more than 3 days)
- Abdominal swelling or pain that doesn’t go away
- Heart palpitations or dizziness after drinking
- Vomiting blood or black, tarry stools
- Confusion or extreme fatigue
These aren’t just side effects. They’re warning signs your body is overwhelmed. Your meds and alcohol are fighting each other-and you’re the one paying the price.
Bottom Line: It’s Not Worth the Risk
Alcohol doesn’t just add to digestive meds-it changes how they work, how your body heals, and how your gut recovers. Even if you’ve done it before without issues, your body changes. Your liver changes. Your meds change. What was safe last year might be dangerous now.
There’s no magic number of drinks that’s “safe.” The only safe choice is to avoid alcohol while you’re treating a digestive issue. Your gut doesn’t need more stress. It needs rest, hydration, and time. And that’s easier to do without alcohol in the mix.






Reviews