When your doctor switches your prescription from a brand-name pill to a generic version, you might feel a flicker of doubt. Generic drugs look different. They cost less. And suddenly, you start wondering: Is this really the same thing? You’re not alone. Millions of people in the U.S. feel this way-even though science says there’s no difference.
The Science Says They’re Identical
Generic drugs aren’t cheap knockoffs. They’re exact copies of brand-name drugs in every way that matters. The FDA requires them to contain the same active ingredient, in the same strength, same dosage form, and same route of administration. That means if you’re taking 25 mg of sertraline for depression, whether it’s Zoloft or the generic, you’re getting 25 mg of sertraline. No more, no less. To get approved, generic manufacturers must prove bioequivalence. That’s a fancy way of saying they have to show the drug gets into your bloodstream at the same rate and to the same level as the brand-name version. The FDA allows a small variation-between 80% and 125% of the brand’s blood concentration. That’s not a loophole. It’s a scientifically accepted range. For most drugs, that tiny difference has zero impact on how well they work. Even for drugs with a narrow therapeutic index-like warfarin or levothyroxine-studies show generics perform just as well when properly manufactured. All facilities making generics, whether in the U.S. or overseas, must follow the same strict manufacturing rules as brand-name makers: Current Good Manufacturing Practices (cGMP). The FDA inspects them. The same way. A 2016 report did find more inspectional observations at foreign plants, but that doesn’t mean the final product is worse. It means inspectors found more paperwork issues, not safety problems. The pills you get at the pharmacy are held to the same standard.Why Do People Think Generics Don’t Work?
If the science is clear, why do so many people believe generics are weaker? It’s not about the drug. It’s about the mind. Look at the packaging. Brand-name drugs come in sleek, colorful boxes with logos you’ve seen on TV. Generics come in plain white bottles with a tiny label. Your brain reads that as “less expensive = less effective.” It’s a visual cue that triggers a psychological response. This isn’t irrational-it’s human. Then there’s the nocebo effect. That’s the opposite of the placebo effect. Instead of feeling better because you believe a treatment works, you feel worse because you believe it won’t. A 2023 JAMA Network Open study showed patients told generics were “equally effective” had 34% better adherence. Those told they were “less effective” had 41% worse adherence. The drug didn’t change. The belief did. Some people report side effects after switching to generics. But in most cases, it’s not the drug-it’s the expectation. When you’re told, “Your doctor switched you to a cheaper version,” your brain starts scanning for anything that feels off. A slight headache. A bit more fatigue. You blame the generic. But if you’d stayed on the brand, you’d have blamed stress, sleep, or the weather.Who’s Most Likely to Doubt Generics?
Not everyone doubts generics equally. Studies show clear patterns. Non-Caucasian patients are significantly more skeptical than white patients. In one 2015 survey, 43% of non-Caucasian respondents questioned whether generics were clinically equivalent, compared to 29% of white respondents. And 56% of non-Caucasian patients asked for brand-name drugs, versus 43% of white patients. Rural communities show even deeper mistrust. In Alabama’s Black Belt region, patients have told pharmacists that generics are “not real medicine,” “for poor people,” or “need higher doses.” These aren’t medical facts-they’re cultural stories passed down. They’re tied to history, distrust in institutions, and economic stigma. Even doctors aren’t immune. One in nine physicians admit they believe generics are less effective. Nearly a third think they cause more side effects. That’s dangerous. When your doctor hesitates, you hesitate. And that hesitation can lead to skipped doses, early discontinuation, or worse health outcomes.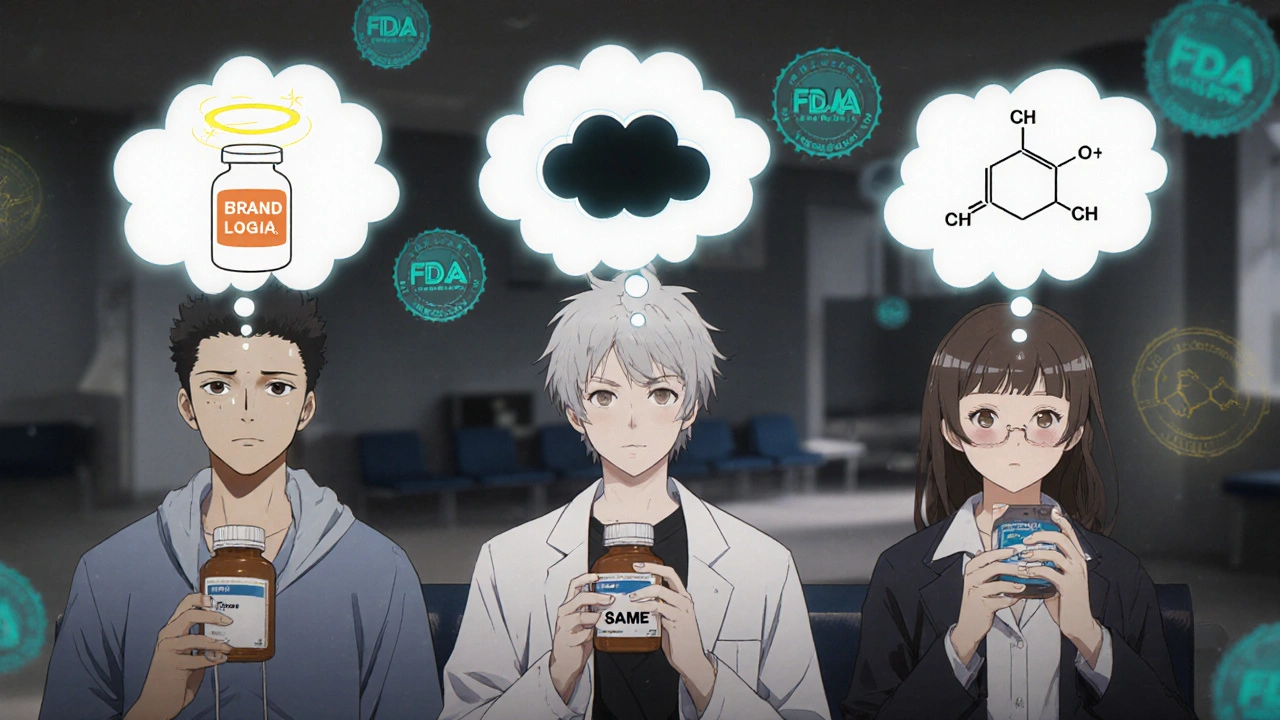
The Real Cost of Doubt
The financial savings from generics are massive. Since 2009, they’ve saved the U.S. healthcare system over $1.7 trillion. In 2022, generics made up 90% of all prescriptions filled. But if everyone believed they worked just as well, savings could jump by another $5.9 billion a year. The bigger cost? Health. A 2019 study found that 22% of patients who thought generics were inferior stopped taking their meds early. That’s more than double the rate of those who had neutral feelings. For someone with high blood pressure, diabetes, or depression, stopping medication isn’t just inconvenient-it’s life-threatening. Brand-name companies know this. They spend $1.8 billion a year on marketing that doesn’t say generics are bad-but makes you feel like they are. Ads that focus on “premium quality,” “clinically proven,” or “trusted by millions” subtly imply generics don’t measure up. They never lie. They don’t have to. Perception does the work for them.What Actually Works to Change Minds
You can’t fix this with a pamphlet. You need direct, clear, and repeated communication. The most effective tactic? Show the patient the active ingredient. “This generic has the same medicine as your old pill-sertraline. Same dose. Same effect.” That alone improves acceptance by 87%, according to a 2022 meta-analysis. Providing FDA documentation helps too. A simple printout from the FDA’s website saying “Generics are required to be as safe and effective as brand-name drugs” gives people something concrete to hold onto. It’s not just a pharmacist’s opinion-it’s the government’s. Addressing the nocebo effect head-on works. Instead of saying, “We’re switching you to a cheaper option,” say, “This is the exact same medicine, just without the brand name. Many people switch and feel no difference at all.” The FDA’s “It’s the Same Medicine” campaign has reached 27 million people since 2019. But only 19% remember it. Why? Because it’s too vague. People don’t remember slogans. They remember conversations.
What You Can Do
If you’ve ever doubted a generic drug, ask yourself: Did you notice a difference before you were told it was generic? Or did the suspicion come after? If you’re switching to a generic, talk to your pharmacist. Ask: “Is this the same active ingredient?” They’ll show you the label. They’ll explain the FDA standards. They’ve seen this happen hundreds of times. If you’re a patient with a chronic condition, keep a symptom journal. Note how you feel before and after the switch. You might be surprised. Most people report no change. A few even feel better-because they’re not stressed about the cost. And if you’re a provider? Don’t assume your patient understands. Don’t just check the box on the substitution form. Spend two minutes explaining. Show them the active ingredient. Say it out loud. That’s the difference between adherence and abandonment.The Bottom Line
Generics aren’t inferior. They’re identical. The difference isn’t in the pill. It’s in the perception. The science is settled. The savings are real. The risks of not taking your medicine? Far greater than any imagined flaw in the generic version. You don’t need to trust the system. You don’t need to trust the brand. You just need to trust the science-and the active ingredient on the label.Are generic drugs really the same as brand-name drugs?
Yes. Generic drugs contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. The FDA requires them to meet the same strict standards for safety, quality, and effectiveness. The only differences are in the inactive ingredients (like fillers or dyes), packaging, and price.
Why do some people feel worse after switching to a generic?
This is usually due to the nocebo effect-where expecting a negative outcome leads to experiencing one. People may feel symptoms because they believe the generic is inferior, not because the drug itself is different. Studies show patients who are told generics are equally effective report better outcomes than those told otherwise.
Are generics less safe than brand-name drugs?
No. All drug manufacturers-brand and generic-must follow the same FDA manufacturing rules (cGMP). Facilities are inspected using the same criteria. The FDA states that generics are as safe and effective as brand-name drugs. Any differences in inspection reports relate to documentation, not product quality.
Can generics cause different side effects?
The active ingredient causes the side effects-and that’s identical in both versions. Minor differences in inactive ingredients can rarely cause reactions in people with specific allergies (like lactose or dyes), but these are not new side effects from the drug itself. If you have a known allergy, check the label or ask your pharmacist.
Why are generics so much cheaper?
Brand-name companies spend billions on research, clinical trials, and marketing to get their drug approved. Generics don’t have to repeat those costs-they just prove they’re equivalent. That’s why they cost 80-85% less. The savings go to patients and the healthcare system, not to profits.
Should I avoid generics for chronic conditions like high blood pressure or thyroid disease?
No. Even for drugs with a narrow therapeutic index-like levothyroxine or warfarin-studies show generics are just as effective and safe. The FDA has additional quality controls for these drugs, and major medical groups like the American College of Clinical Pharmacy confirm their equivalence. Consistency matters more than brand-stick with the same generic manufacturer if you notice stability.
How can I be sure the generic I’m getting is approved by the FDA?
All legally sold generics in the U.S. must be FDA-approved. Look for the drug name on the bottle-it should match the brand-name drug exactly. You can also check the FDA’s online database of approved generics. If a pharmacy sells a drug labeled as generic without FDA approval, it’s illegal.





Reviews
Man, I used to think generics were just placebo pills in disguise until my cousin in Dublin got prescribed generic sertraline and saved like $200 a month. Same bottle, same effects. Honestly, the only thing different was the price and the fact that I stopped hearing her complain about her bills. The brain is a weird thing-makes you feel like cheaper means worse, but your body doesn’t care what the label looks like.
My grandma switched from brand-name Lipitor to generic and thought she was getting scammed. Told her it’s literally the same chemical. She still didn’t believe it until I printed out the FDA page showing the equivalence standards. Now she’s the one pushing everyone else to switch. People don’t distrust the science-they distrust the system. Show them the paper, not the pitch.
It is imperative to recognize that the perception gap surrounding generic medications is deeply rooted in socio-economic narratives and historical mistrust within marginalized communities. The clinical equivalence of generics is not merely a regulatory assertion-it is a scientifically validated fact, supported by rigorous bioequivalence testing and post-market surveillance. Healthcare providers must engage in deliberate, culturally competent communication to dismantle these misconceptions, ensuring that patients are not penalized for systemic inequities through non-adherence.
So many people don’t realize that the only real difference is the color of the pill and the price tag 😊 I had a patient tell me last week that her generic blood pressure med made her ‘feel weird’-turned out she’d been stressed about the switch and blamed the pill. We sat down, read the label together, and she realized it was the same exact ingredient. She’s been fine since. Sometimes all it takes is pointing to the active ingredient and saying ‘this is it.’
Generic = same active ingredient. Period. 🧪 The FDA doesn’t cut corners. If you’re feeling off after switching, it’s not the drug-it’s your brain playing tricks. I’ve seen this a hundred times in the clinic. Just show the patient the label. They’ll calm right down. Also, side note: generics saved my dad’s life. He couldn’t afford brand-name insulin. Don’t let marketing scare you.
There’s a reason brand-name companies spend billions on ads that never mention generics by name. They don’t need to say ‘our drug is better.’ They just need to make you feel like you’re getting premium quality. And that’s enough. The real issue isn’t science-it’s branding. We’ve been trained to equate cost with value. That’s not medical thinking. That’s consumer psychology. And it’s working.
Generics are government-approved junk for poor people. You think the FDA cares about you? They just want to save money. Your ‘science’ is a lie. I’ve seen people get sicker after switching. Trust me, I know.
It’s worth noting that the FDA’s bioequivalence standards are among the most stringent in the world. A 2019 meta-analysis of over 500 studies found no clinically significant difference in outcomes between generics and brand-name drugs across 12 therapeutic categories. Even for narrow-therapeutic-index medications like warfarin, adherence rates and clinical outcomes were statistically identical. The perception of inferiority is a cultural artifact, not a pharmacological reality.