When your liver is damaged, especially from cirrhosis, blood can't flow through it the way it should. This forces blood to find other routes, building up pressure in the portal vein-the main vessel that carries blood from your intestines to your liver. That pressure is called portal hypertension. It doesn’t cause symptoms on its own, but it sets off a chain reaction that can turn deadly. Varices, ascites, and other complications don’t just appear out of nowhere-they’re direct results of this rising pressure. And if you’re living with cirrhosis, you’re at serious risk.
What Exactly Is Portal Hypertension?
Portal hypertension isn’t a disease on its own. It’s a consequence. The normal pressure in the portal vein is between 5 and 10 mmHg. Once it climbs above 10 mmHg-or when the hepatic venous pressure gradient (HVPG) hits 5 mmHg or higher-you’ve crossed into portal hypertension. The HVPG is the gold standard measurement, taken during a minor procedure where a catheter is inserted into a liver vein. It’s invasive, but it’s the most accurate way to know how bad things are.About 90% of cases come from cirrhosis. That’s when scar tissue replaces healthy liver cells, blocking blood flow. The remaining 10% are non-cirrhotic, caused by things like blood clots in the portal vein or rare conditions like schistosomiasis. But no matter the cause, the result is the same: blood backs up, pressure rises, and your body tries to compensate in dangerous ways.
Varices: The Time Bomb in Your Esophagus
As pressure builds, blood looks for escape routes. The weakest spots? The veins in your esophagus and stomach. These veins stretch, swell, and become varices-like bulging, fragile balloons. About half of people with cirrhosis develop them within 10 years.Here’s the scary part: if one of these varices bursts, you can vomit liters of blood in minutes. The first bleed kills 15-20% of people within six weeks. Even if you survive, the chance of bleeding again within a year is 60% without proper treatment.
Doctors don’t wait for a bleed to happen. If you have cirrhosis, you get screened with an endoscopy. If medium or large varices are found, you’re put on a non-selective beta-blocker like propranolol. The goal? Lower your heart rate by 25% or hit a daily dose of 160 mg. This reduces pressure in the portal system and cuts your first bleeding risk by nearly half.
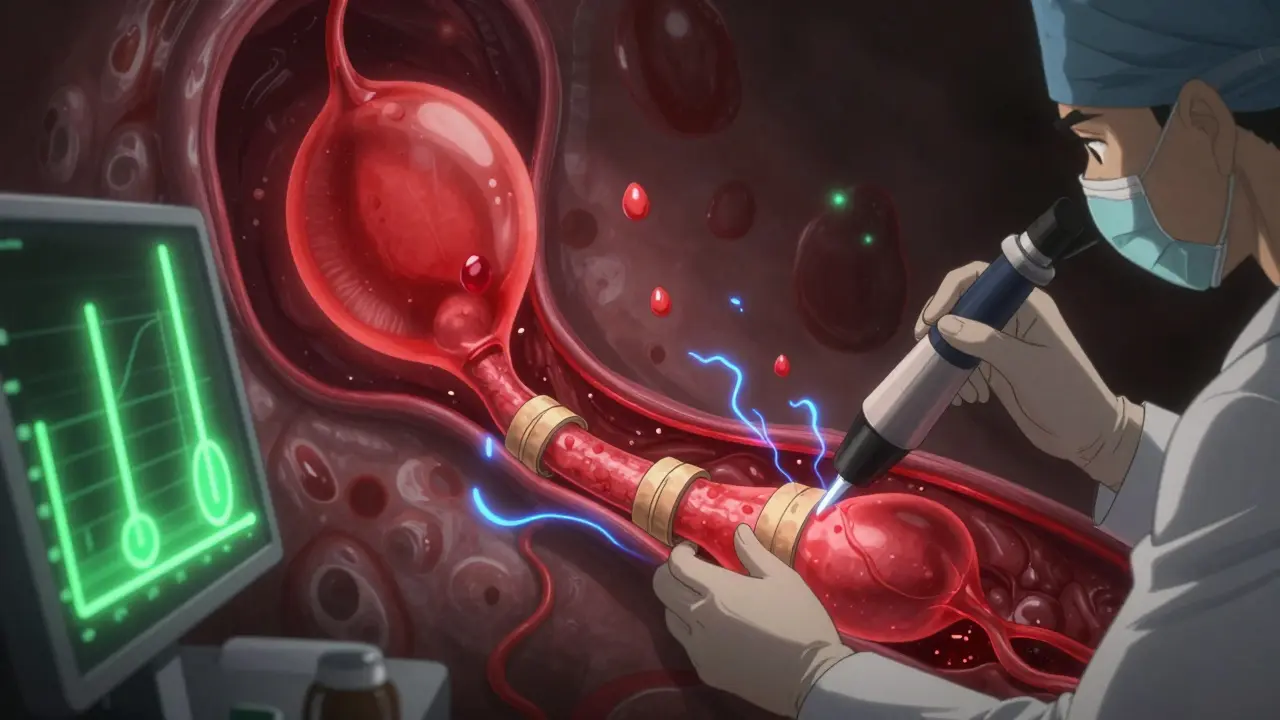
If you’ve already bled, it’s a medical emergency. You need endoscopic band ligation within 12 hours-where tiny rubber bands are placed around the varices to cut off blood flow. This cuts rebleeding rates from 60% down to 20-30%. Antibiotics like ceftriaxone are given immediately to prevent deadly infections. Vasoactive drugs like terlipressin or octreotide are used to squeeze the blood vessels and slow the bleeding until the endoscopy can be done.
Ascites: When Your Belly Swells Like a Water Balloon
Another major complication? Ascites-fluid leaking into your abdomen. It happens in 60% of cirrhotic patients within 10 years. Why? The liver stops making enough albumin, a protein that keeps fluid in your blood vessels. With low albumin and high pressure, fluid oozes out into your belly.At first, it’s just a feeling of fullness. Then your belly gets big. You get short of breath. You can’t tie your shoes. Some people lose their jobs because they can’t stand for more than 20 minutes. One patient on a liver forum described it as “having a tire iron in your abdomen.”
First-line treatment is simple but strict: no salt. Less than 2,000 mg a day. Then diuretics-spironolactone (100 mg daily) and sometimes furosemide (40 mg). Together, they pull fluid out through your kidneys. For most people, this works. But if the fluid keeps coming back despite treatment, you have refractory ascites.
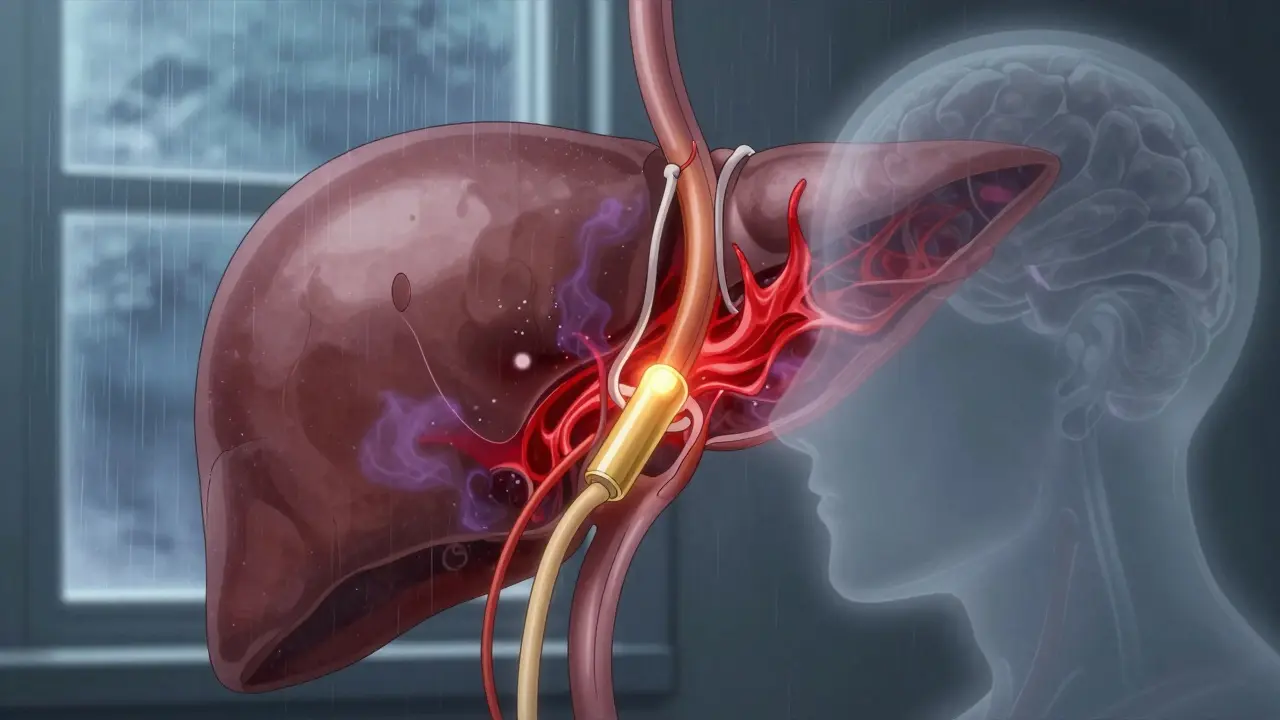
When that happens, doctors drain the fluid with paracentesis. It’s quick, but it’s not a cure. Every liter removed needs 8 grams of albumin replaced to keep your blood pressure stable. If you need it more than twice a week, you’re at high risk. That’s when TIPS-transjugular intrahepatic portosystemic shunt-comes in.
TIPS is a procedure where a stent is placed between a liver vein and a vein going to the heart. It creates a shortcut, lowering pressure in the portal system. Success rate? 90-95%. But here’s the trade-off: 20-30% of patients develop hepatic encephalopathy-brain fog, confusion, even coma-because toxins that used to be filtered by the liver now bypass it.
The Hidden Threats: Encephalopathy and Kidney Failure
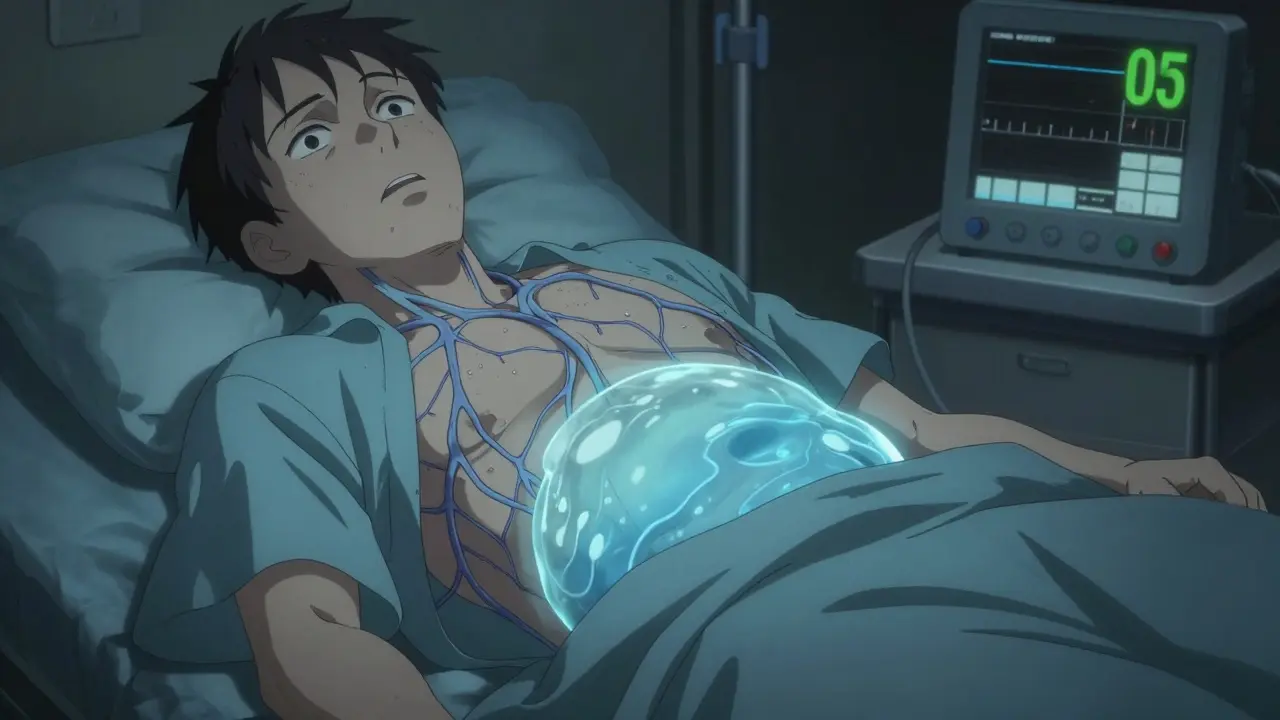
Portal hypertension doesn’t stop at varices and ascites. It strains your whole body. About 40% of cirrhotic patients develop hepatic encephalopathy. It starts with mild forgetfulness, then mood swings, then slurred speech. It’s caused by ammonia and other toxins building up because the liver can’t clean them.Then there’s hepatorenal syndrome-a type of kidney failure that happens in 18% of hospitalized cirrhotic patients with ascites. Your kidneys shut down not because they’re damaged, but because your body redirects blood away from them to protect your brain and heart. It’s a death sentence without a transplant.
There’s no magic drug for either. Rifaximin helps with brain fog. Albumin and vasoconstrictors like midodrine can help with kidney function, but they’re temporary fixes. The only real solution? A liver transplant.
What’s Changing in Treatment?
The field is evolving fast. Five years ago, we relied on HVPG measurements to guide treatment. Now, non-invasive tools like spleen stiffness elastography are hitting 85% accuracy. You can get the same info without a catheter. In September 2023, Europe approved the Hepatica SmartBand-a wearable device that estimates portal pressure using bioimpedance. It’s not perfect, but it’s a game-changer for monitoring.Drug development is also picking up. Simtuzumab, a new antibody targeting liver scarring, showed a 35% drop in portal pressure in phase 3 trials. Twelve other drugs are in phase 2 testing, aiming to reduce pressure without dropping blood pressure too low-a common side effect of current meds.
AI is helping too. Mayo Clinic’s algorithm predicts variceal bleeding with 92% accuracy by analyzing scans, lab values, and patient history. That means we can spot high-risk patients before they bleed.
Why So Many Patients Still Die
Despite all this, mortality from variceal bleeding hasn’t improved much in 40 years. Why? Because treatment is reactive, not preventive. Most patients don’t get regular endoscopies. Beta-blockers are underused because of side effects-fatigue, dizziness, low heart rate. Many are scared of TIPS because of encephalopathy. And liver transplants? The wait in the U.S. is 14 months on average.Non-cirrhotic portal hypertension adds another layer. If you have a portal vein clot, beta-blockers won’t help. You need anticoagulants to dissolve the clot. Get it wrong, and you bleed.
And let’s not forget the human cost. Patients report cognitive side effects from beta-blockers. The constant fear of bleeding. The exhaustion from paracentesis. The isolation. One Reddit user said, “I live with the terror of vomiting blood again.” That’s not just a symptom-it’s a life sentence.
What You Can Do
If you have cirrhosis or know someone who does:- Get screened for varices with endoscopy-don’t wait for symptoms.
- If prescribed a beta-blocker, take it daily. Don’t skip doses because you feel tired.
- Stick to a low-sodium diet. Read labels. Avoid processed food, canned soups, soy sauce.
- Know the signs of bleeding: black stool, vomiting blood, dizziness, fainting. Call 911.
- Ask about non-invasive pressure testing. Ask if you’re a candidate for TIPS.
- Consider transplant evaluation early. Don’t wait until you’re in crisis.
Portal hypertension isn’t curable yet. But it’s manageable-if you act early, stay consistent, and work with a liver specialist. The tools are here. The knowledge is here. What’s missing is the urgency.
What is the normal portal vein pressure?
Normal portal vein pressure is between 5 and 10 mmHg. Portal hypertension is diagnosed when pressure exceeds 10 mmHg, or when the hepatic venous pressure gradient (HVPG) is 5 mmHg or higher. Clinically significant portal hypertension is defined as HVPG ≥10 mmHg.
Can portal hypertension be cured?
No, portal hypertension itself cannot be cured unless the underlying cause is reversed-like removing a blood clot or curing hepatitis. In cirrhosis, the scarring is permanent. Treatment focuses on lowering pressure, preventing complications, and managing symptoms. Liver transplant is the only cure for advanced cases.
What are the first signs of varices?
Varices usually have no symptoms until they bleed. That’s why screening is critical. If they rupture, symptoms include vomiting bright red blood, passing black tarry stools, dizziness, rapid heartbeat, and fainting. These are medical emergencies.
How do you treat ascites at home?
At home, treat ascites with strict sodium restriction (under 2,000 mg/day), daily diuretics like spironolactone, and monitoring your weight. Weigh yourself every morning. A sudden gain of 2 kg (4.4 lbs) in a day means fluid is building up. Avoid alcohol, and take medications exactly as prescribed. Never drain fluid yourself-this must be done by a doctor.
Is TIPS dangerous?
TIPS is effective but carries risks. About 20-30% of patients develop hepatic encephalopathy within a year. There’s also a small risk of infection, bleeding, or stent blockage. But for patients with refractory ascites or repeated bleeding, the benefits often outweigh the risks. It’s not a first-line treatment-it’s reserved for when other options fail.
Can non-cirrhotic portal hypertension be treated differently?
Yes. If portal hypertension is caused by a blood clot in the portal vein, beta-blockers won’t help. Instead, anticoagulants like warfarin or direct oral anticoagulants are used to dissolve the clot. The treatment depends entirely on the cause-so accurate diagnosis is essential.
How often should I get screened for varices?
If you have cirrhosis and no varices, get an endoscopy every 2 years. If you have small varices, check every 1-2 years. If you’ve had a bleed, you need endoscopy every 6 months for the first year, then annually if stable. Always follow your hepatologist’s advice-timing can save your life.



Reviews
Just had my third paracentesis this month. They tell me to cut salt, but when you’re living on ramen because it’s all you can afford, what’s the point? I’m tired of being told to ‘just take better care of myself’ while my insurance denies TIPS.
I’m from India and I’ve seen so many patients here with portal hypertension who never even heard of HVPG until they were vomiting blood. No screening, no beta-blockers, just folk remedies and prayers. The system here is broken. We need outreach programs, not just fancy gadgets like the Hepatica SmartBand that no one can afford. My cousin died last year because his doctor said ‘come back in six months’-he didn’t make it to the next appointment.
It’s not just about medicine-it’s about dignity. People shouldn’t have to choose between food and spironolactone.
Let’s be real-90% of these patients are alcoholics who ignored warnings for 15 years. Now they want a transplant like it’s a free Uber ride. I’ve worked in hepatology for 12 years. The ones who survive? They quit drinking. The rest? They blame the system. Wake up. Prevention isn’t optional. It’s non-negotiable.
Hi, I’m a nurse who works with cirrhosis patients daily. Just wanted to say: if you’re on propranolol and feel dizzy, don’t stop it-call your doc. We can adjust the dose. And yes, the fatigue sucks, but it’s better than bleeding out in the ER. Also, low sodium doesn’t mean no flavor-try lemon, herbs, garlic powder. I have a free PDF guide if anyone wants it.
My aunt got TIPS last year. She’s been fine for 11 months-no more ascites, no more hospital visits. But she gets confused sometimes. We thought it was aging. Turns out it’s hepatic encephalopathy. Now we give her lactulose twice a day. It’s not perfect, but it’s a gift. Don’t be scared of TIPS. Be scared of doing nothing.
To anyone reading this: you are not alone. I’ve been where you are-afraid to sleep, terrified of the next meal, wondering if today’s the day my belly explodes or I wake up choking on blood. But I’m alive. I’m on propranolol, I track my sodium like a hawk, and I got on the transplant list at 42. It took 10 months. I’m waiting. And I’m still here. You can be too. Not because you’re strong-because you deserve to be.
Okay but like… have y’all seen the new AI algorithm from Mayo? 😱 92% accuracy?? Like… I just got my scan results and it flagged me as high risk. I cried. Then I called my hepatologist. We’re doing banding next week. This tech? It’s real. It’s saving lives. 🙏 #portalhypertensionwarrior
Oh please. You all act like this is some new epidemic. People have been dying from cirrhosis since the 1950s. You want a cure? Stop drinking. Stop eating processed crap. Stop blaming doctors. The tools are here. The knowledge is here. You just don’t want to change. That’s not a medical problem-that’s a moral one.
There’s a quiet kind of courage in taking your beta-blocker every day when you’re tired. In weighing yourself at 6 a.m. when you’re depressed. In saying ‘no’ to that salty snack even when no one’s watching. That’s not weakness. That’s the daily grind of survival. And it deserves more than pity-it deserves recognition.
Non-cirrhotic portal hypertension is underdiagnosed. I had a patient with portal vein thrombosis from protein S deficiency. Beta-blockers made him worse. Anticoagulation saved him. Always test the cause. Don’t assume.
Why are we still using HVPG as gold standard in 2024? It’s invasive, expensive, and inaccessible. We have ultrasound elastography that’s 85% accurate and costs $200. Why aren’t hospitals switching? Profit. It’s always profit.
Anyone who says ‘I can’t afford the diet’ is making excuses. You can’t afford not to. One bag of chips = 500mg sodium. That’s 25% of your daily limit. You think the ER bill is cheaper? Wake up. This isn’t about money-it’s about priorities.
Let’s not romanticize this. TIPS isn’t a miracle. It’s a trade-off: ascites gone, brain fog everywhere. Patients are left confused, angry, and isolated. And we call it ‘success’? We’re not curing disease-we’re just delaying death with side effects. Someone needs to ask: is this living, or just not dying yet?
My mom got her transplant last year. She’s alive. But the waiting list? It’s a lottery. And if you’re over 65? Good luck. They say ‘you’re not sick enough yet’-but you’re only sick enough when you’re already dying. That’s the system.
Thank you for this comprehensive overview. As a healthcare administrator, I’m working to implement standardized screening protocols in our regional clinics. Early detection saves lives-and money. We’re piloting non-invasive elastography next quarter. Stay hopeful.