Prepare for Medication Review: What You Need to Know Before Your Appointment
When you prepare for medication review, a structured evaluation of all the drugs you’re taking to ensure they’re still safe and necessary. Also known as medication reconciliation, it’s not just a formality—it’s a chance to stop taking pills that don’t help, cut out dangerous combos, and save money. Many people take five or more medications, and that’s where things get risky. A single interaction between your blood pressure pill and a common supplement can send you to the ER. The goal isn’t to remove everything—it’s to make sure every drug still earns its place in your daily routine.
Doctors and pharmacists don’t guess what you’re taking. They rely on what you tell them. That’s why writing down every pill, patch, vitamin, and herbal tea matters. Don’t forget the over-the-counter stuff—like ibuprofen, antacids, or sleep aids. These often slip through the cracks. One study found that nearly 40% of older adults had at least one unnecessary or unsafe medication in their routine, and most didn’t realize it. The drug interactions, harmful effects that happen when two or more substances react inside your body. Also known as medication conflicts, they’re the silent threat behind falls, confusion, and hospital stays. Think of it like a recipe: adding too many spices ruins the dish. Your body isn’t designed to handle 10 different chemicals at once without something going wrong.
Another big piece is deprescribing, the careful process of stopping medications that no longer help or may be doing more harm than good. Also known as medication reduction, it’s not about quitting cold turkey—it’s about smart, step-by-step removal under supervision. If you’ve been on a sedative for years because you "couldn’t sleep," but now you’re dizzy and falling, that’s a red flag. Same with long-term painkillers that stopped working but you keep taking anyway. The pharmacy consultation, a direct conversation with a pharmacist about your full drug list to spot risks and alternatives. Also known as medication therapy management, it’s often free with your insurance and happens before your doctor even sees you. They’ll catch things your doctor missed—like how your antihistamine makes your glaucoma worse, or how your calcium supplement blocks your thyroid medicine.
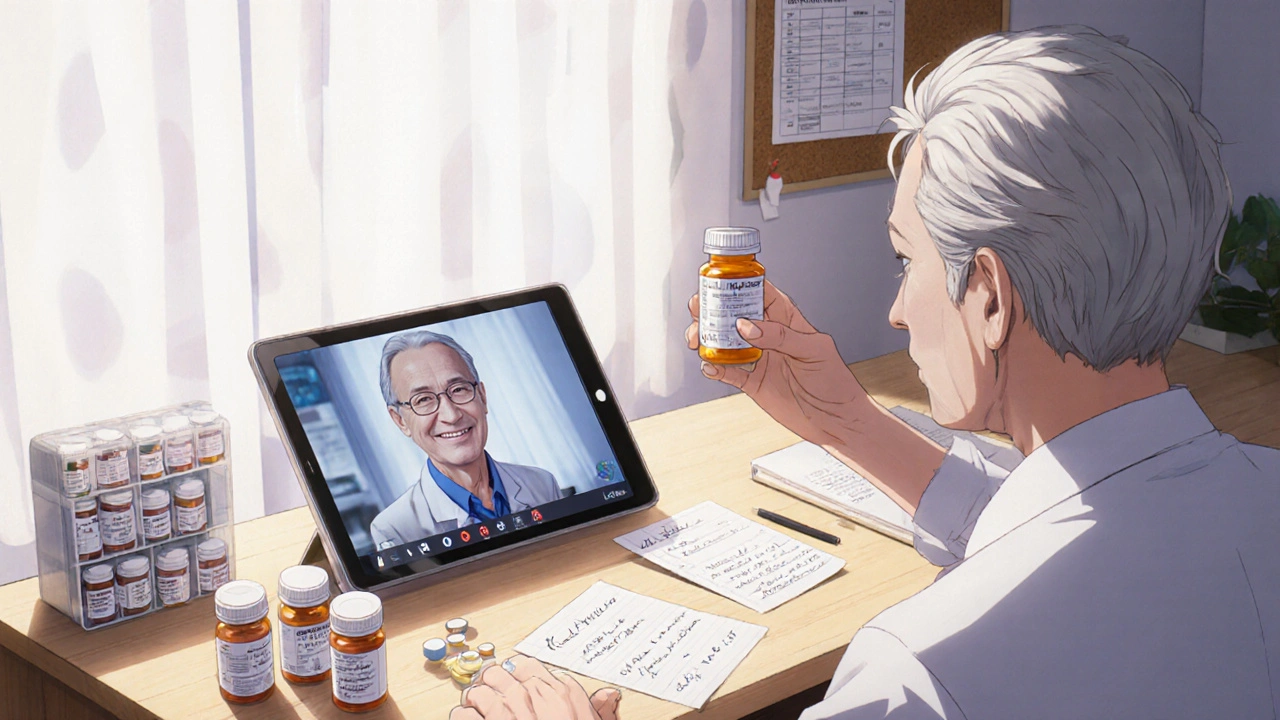
Bring your actual bottles—not just a list. Labels show dosages, expiration dates, and why the drug was prescribed. If you don’t know why you’re taking something, say so. That’s the whole point of the review. You’re not being judged—you’re being protected. This isn’t just for seniors. Anyone on multiple prescriptions, especially after a hospital stay or a new diagnosis, should do this at least once a year.
What you’ll find in the posts below are real examples of how medication reviews change lives. From spotting dangerous alcohol-drug combos to realizing your "essential" painkiller is making your stomach bleed. You’ll learn how to talk to your doctor without sounding confrontational, how to tell if a drug is still working, and why some meds should be dropped even if they "always worked before." This isn’t theory. It’s what people actually do when they take control of their own health.