Antibiotic Liver Injury Risk Calculator
This tool estimates your risk of developing liver injury from antibiotics based on your medication and health factors. Results are for informational purposes only.
Antibiotics save lives. But for some people, the very drugs meant to fight infection can quietly damage the liver-sometimes without warning. This isn’t rare. In fact, antibiotics cause 64% of all drug-induced liver injury cases in intensive care units. That’s more than any other class of medication. And while most people take antibiotics without issue, a small but significant number develop hepatitis (liver inflammation) or cholestasis (bile flow blockage) as a side effect. Understanding how this happens, who’s at risk, and what to watch for can make all the difference.
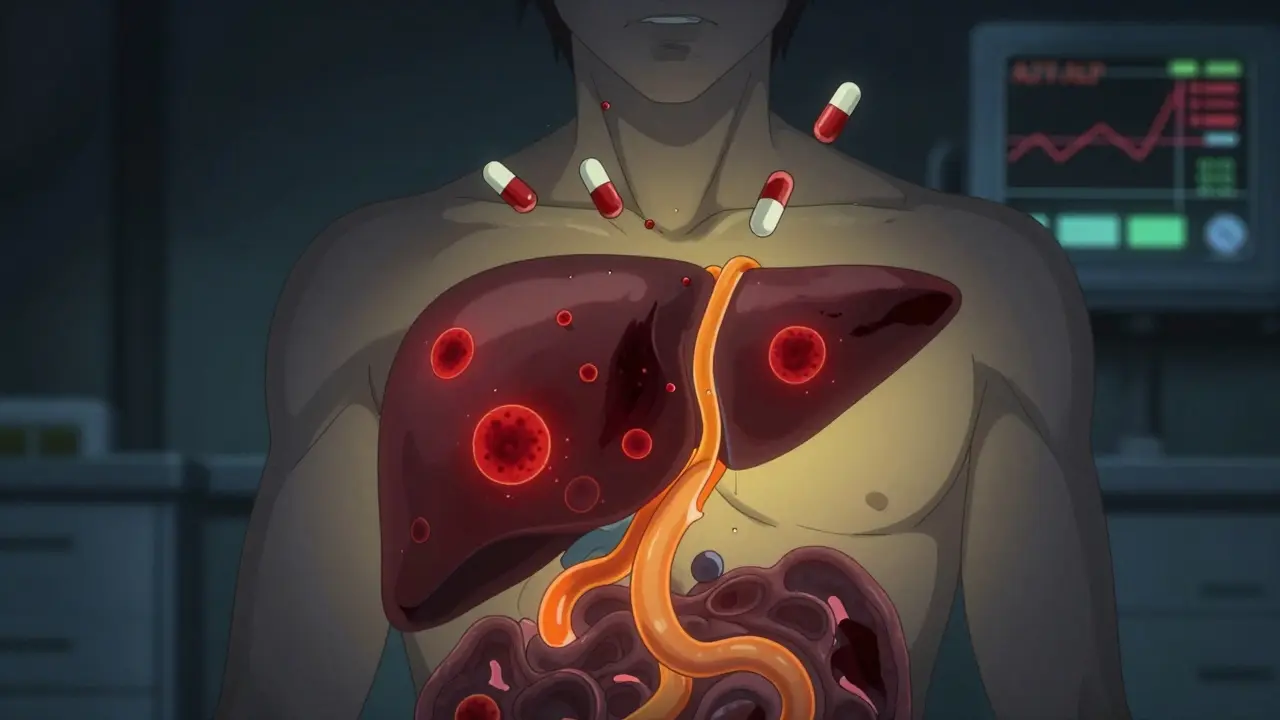
How Antibiotics Hurt the Liver
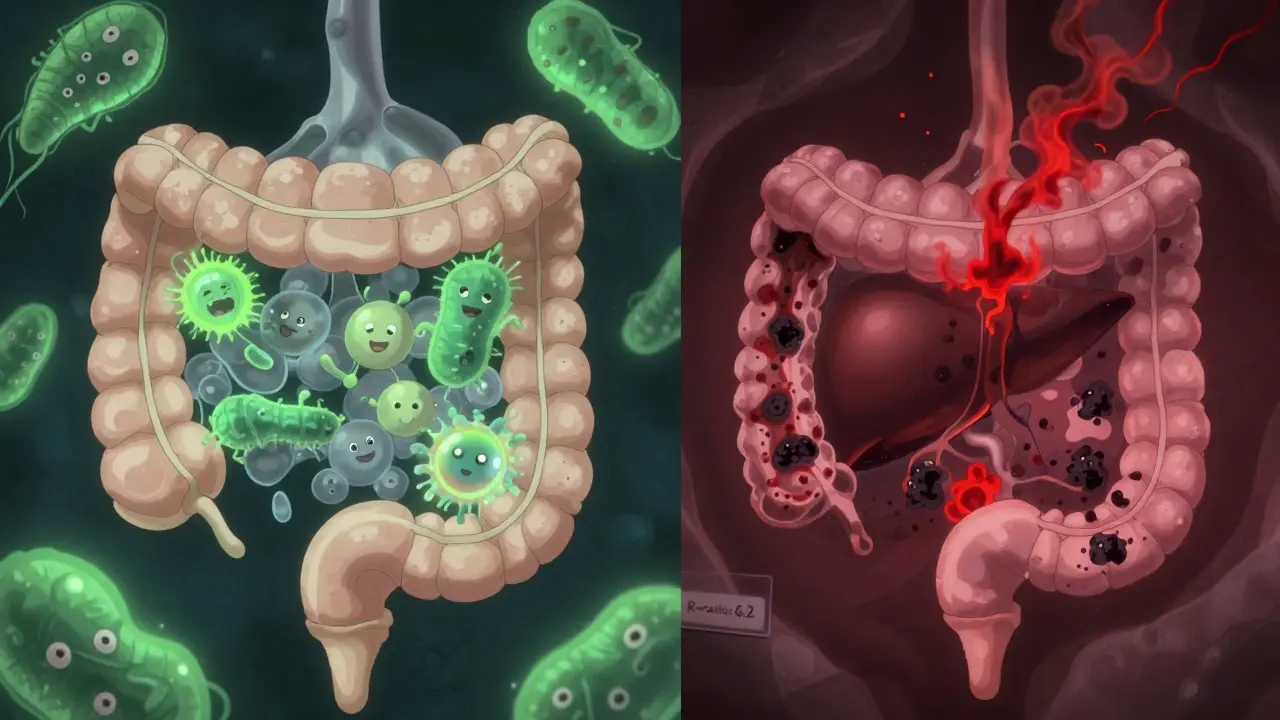
It’s not just one mechanism. Antibiotics damage the liver in multiple ways, often at the cellular level. Some interfere with mitochondria-the energy factories inside liver cells-slowing down fat burning and causing toxic buildup. Others create reactive chemicals during metabolism that directly attack liver tissue. And then there’s the gut connection: antibiotics wipe out good bacteria, letting harmful ones take over. This disrupts the gut barrier, letting toxins leak into the bloodstream and reach the liver, triggering inflammation.
The result? Two main patterns show up in blood tests. One is hepatocellular injury, where liver cells die off, causing ALT (alanine aminotransferase) levels to spike above 5 times the normal limit. The other is cholestatic injury, where bile can’t flow properly, pushing ALP (alkaline phosphatase) levels above 2 times normal. Sometimes, you get both-a mixed pattern. Doctors use something called the R-ratio to tell them which is which: R > 5 means hepatitis; R < 2 means cholestasis; R between 2 and 5 means mixed.
Which Antibiotics Are Most Likely to Cause Trouble?
Not all antibiotics are created equal when it comes to liver risk. Some are far more dangerous than others.
- Amoxicillin-clavulanate (Augmentin) is the biggest offender. It causes cholestatic injury in 70-80% of cases. About 15-20 people out of every 100,000 who take it develop liver injury. Symptoms often appear 1-6 weeks after starting the drug.
- Tazobactam/piperacillin (Zosyn) is especially risky in hospitals. One study found nearly 29% of ICU patients on this combo for over 7 days developed liver injury-more than double the rate seen with meropenem.
- Fluoroquinolones like ciprofloxacin and azithromycin tend to cause mixed injury. They’re faster-acting, with liver damage sometimes showing up in just 1-2 weeks.
- Rifampin causes dose-dependent toxicity. Higher doses = higher risk. And when combined with isoniazid (used for tuberculosis), the risk multiplies.
Even antibiotics considered "safe" can cause problems in the wrong person. Nitrofurantoin and trimethoprim-sulfamethoxazole fall into the moderate-risk category. And here’s something surprising: men are 2.4 times more likely than women to develop liver injury from meropenem. Why? Researchers aren’t sure yet-but genetics might be involved.
Who’s Most at Risk?
It’s not just about the drug. Your body’s condition matters just as much.
- Long courses: Taking antibiotics for 7 days or more increases liver injury risk by over 3 times.
- Sepsis: If you’re already fighting a severe infection, your liver is under stress. Sepsis alone makes antibiotic-related liver injury 1.8 times more likely.
- Genetics: Certain HLA gene variants make some people far more susceptible to idiosyncratic reactions-meaning their immune system mistakenly attacks the liver after the drug is processed. This isn’t predictable by standard tests.
- Age and existing liver disease: Older adults and those with fatty liver, hepatitis B, or alcohol-related damage are more vulnerable.
- Multiple drugs: Taking antibiotics with other liver-metabolized meds (like statins or seizure drugs) raises the risk.
And here’s the hard part: in ICU patients, liver enzyme spikes are common. But are they from the antibiotic? From septic shock? From low blood pressure? From another drug? It’s often impossible to tell without ruling out everything else.
What Are the Symptoms?
Some people feel nothing at all. Their only sign is an abnormal blood test. But others develop clear symptoms:
- Jaundice (yellow skin or eyes)
- Dark urine
- Light-colored stools
- Unexplained nausea or vomiting
- Loss of appetite
- Extreme fatigue
- Abdominal pain, especially on the right side
These signs usually appear days to weeks after starting the antibiotic. In rare cases, liver injury can progress to acute liver failure-especially with amoxicillin-clavulanate. That’s why early detection matters.
How Do Doctors Diagnose It?
There’s no single test. Diagnosis is a process of elimination.
- Baseline LFTs: Before starting high-risk antibiotics like Augmentin, doctors should check liver enzymes.
- Repeat testing: For high-risk drugs, check again after 1-2 weeks. For ICU patients on long courses, test weekly.
- Calculate the R-ratio: This tells you if the injury is hepatocellular, cholestatic, or mixed.
- Rule out other causes: Viral hepatitis, gallstones, alcohol, autoimmune disease-all need to be checked.
- Use LiverTox: The National Institute of Diabetes and Digestive and Kidney Diseases maintains a free, updated database of over 600 medications and their liver risks. Doctors use it daily.
There’s no magic number for when to stop the drug. The general rule? Discontinue if ALT is over 5× ULN, or if ALP is over 2× ULN and you have symptoms. But in critically ill patients, sometimes the benefit of continuing the antibiotic outweighs the risk.
What Happens After Stopping the Antibiotic?
Most people recover fully once the drug is stopped. Liver enzymes usually return to normal within 2-8 weeks. But recovery isn’t guaranteed.
- Cholestatic injury often takes longer to resolve-sometimes months.
- Severe cases can lead to chronic liver damage or even require a transplant.
- Some people develop a lasting sensitivity to that antibiotic. Re-exposure can cause a faster, more severe reaction.
There’s no specific antidote. Supportive care-hydration, rest, avoiding alcohol and other liver stressors-is the main treatment. Steroids? Only in rare autoimmune-like cases. And never restart the offending antibiotic unless absolutely necessary-and even then, with extreme caution.

Can You Prevent It?
Yes, to some extent.
- Use antibiotics only when needed. Many respiratory infections are viral. Antibiotics won’t help-and they might hurt your liver.
- Keep courses short. If 5 days works, don’t give 10.
- Monitor high-risk patients. Elderly, septic, or those on multiple meds need closer LFT checks.
- Consider alternatives. For example, if someone has a history of liver issues, avoid amoxicillin-clavulanate. Use a different class.
And the future? Researchers are looking at gut microbiome testing. Early data shows that people with low levels of Faecalibacterium prausnitzii are nearly 4 times more likely to develop liver injury from antibiotics. A simple stool test might one day tell your doctor which antibiotic is safest for you.
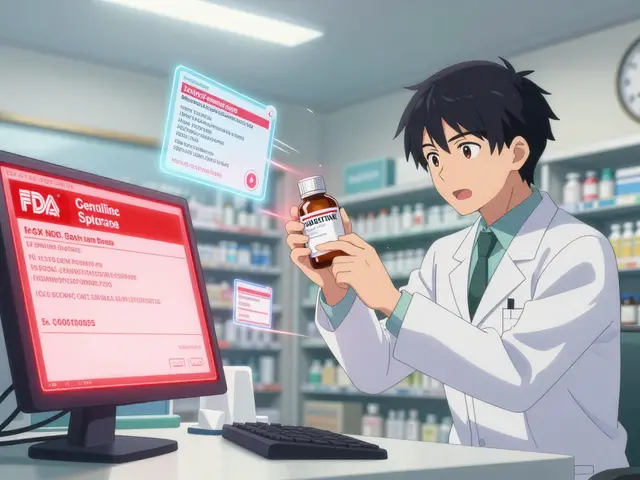
What’s Being Done to Fix This?
The problem is big enough that regulators are paying attention.
- The FDA has issued 17 safety alerts on antibiotic liver injury since 2010.
- The EMA updated its guidelines in March 2023 to include specific monitoring for new β-lactam combinations.
- Clinical trials are testing probiotics to protect the gut microbiome during antibiotic therapy. Early results look promising.
- Pharmaceutical companies now screen new antibiotics for mitochondrial toxicity and bile pump inhibition before they even reach humans. It’s slowed drug development-but saved lives.
And in the next 5-7 years, pharmacogenomics could change everything. If your HLA profile shows high risk for certain drugs, your doctor might avoid prescribing them entirely. Personalized antibiotic therapy isn’t science fiction anymore-it’s coming.
Bottom Line
Antibiotics are essential. But they’re not harmless. Liver injury from these drugs is common, often silent, and sometimes serious. The key is awareness. If you’re prescribed a long course of antibiotics-especially Augmentin, Zosyn, or a fluoroquinolone-ask your doctor: "Should I get my liver checked?" If you’re in the hospital and your bilirubin or enzymes rise, don’t assume it’s just "the infection." Push for answers.
Most people recover. But recovery starts with catching it early. Know the signs. Know the risks. And never underestimate the power of a simple blood test.



Reviews
Man, I had no idea antibiotics could wreck your liver like that. I’ve taken Augmentin three times for sinus infections and never thought twice. Guess I’ll ask my doc to check my LFTs next time.
OMG this is so important!! I had a friend who got jaundice after Zosyn and they thought it was just ‘the flu’ for weeks!! Why isn’t this on every prescription label??
Given the pharmacokinetic profile of β-lactam/β-lactamase inhibitor combinations, the hepatotoxic potential is directly proportional to duration of exposure and baseline hepatic reserve. The R-ratio methodology, while clinically useful, lacks sensitivity for subclinical mitochondrial dysfunction. I recommend preemptive mitochondrial DNA quantification in high-risk cohorts.
Interesting how the gut-liver axis plays into this. I’ve been taking probiotics after every antibiotic since my last bout of C. diff. Never thought about liver protection, but now I’m wondering if that’s helping more than I knew.
This gave me chills 😢 I’m so glad I got my liver checked after my last round of cipro. Normal. But I never would’ve known if I hadn’t read this. Thanks for sharing. 🙏
Of course the FDA issued 17 safety alerts. But they still allow these drugs to be sold over the counter in 37 states. The system is broken. People die because corporations prioritize profit over patient safety. This isn’t an accident-it’s negligence.
Hey everyone-this is such a critical conversation. I’m a nurse in the ICU and I see this all the time. We check LFTs weekly on anyone on Zosyn longer than 5 days. It’s not routine everywhere, but it should be. Don’t be afraid to ask your team: ‘Are we monitoring for drug-induced liver injury?’ You’re not being annoying-you’re saving your own life.
While the data presented is compelling, one must consider the broader context of public health. Antibiotics are indispensable in modern medicine. To overemphasize rare adverse effects risks undermining public compliance with life-saving regimens. A balanced approach is required-not alarmism.
It’s fascinating how medicine is moving toward personalized risk assessment. We used to treat the drug as the variable. Now we’re learning the person is the variable. If our genes determine whether a drug becomes a toxin, then perhaps the future of prescribing isn’t about what’s safest for most-but what’s safest for you.
It is worth noting that the assertion regarding the 64% statistic for antibiotic-induced liver injury in intensive care units is derived from a single-center retrospective cohort study with a sample size of 217 patients, published in the Journal of Hepatology in 2021. While statistically significant within its parameters, extrapolation to general populations may introduce selection bias. Furthermore, the R-ratio’s diagnostic utility is contingent upon accurate baseline enzyme values, which are frequently unavailable in emergent settings. The clinical applicability of the proposed screening protocols is therefore limited by real-world constraints of resource allocation and time-sensitive decision-making in critical care environments.