When a child has asthma, their airways get tight and swollen, making it hard to breathe. It’s not just about coughing or wheezing - it’s about daily life. School, sports, sleep, even playing with friends can all be affected. But here’s the good news: with the right tools and a clear plan, most kids with asthma can live full, active lives. The key? Spacers, smart school policies, and a personalized asthma care plan.
Why Spacers Are Non-Negotiable for Kids
A spacer isn’t just a plastic tube you attach to an inhaler. It’s the difference between medicine landing in the back of the throat - where it does nothing - and getting deep into the lungs, where it actually helps. For children, especially those under five, using an inhaler alone is nearly impossible. They can’t coordinate pressing the puff and breathing in at the same time. That’s where spacers come in. Spacers hold the medicine after you press the inhaler, giving the child time to breathe it in slowly and naturally. Studies show that when used correctly, spacers deliver 73% more medication to the lungs than inhalers alone. This means fewer symptoms, fewer emergency visits, and less risk of side effects like hoarseness or thrush. The science is clear: the American Academy of Pediatrics and Global Initiative for Asthma (GINA) both say spacers should be used with every inhaler for every child. And it’s not just theory - real-world data backs it up. One JAMA Pediatrics study found that kids using spacers had a 5% hospital admission rate for asthma attacks, compared to 20% for those using nebulizers. That’s a 75% drop. But here’s the catch: spacers only work if they’re used right. A 2022 study found that only 54% of children using spacers without a mask got the full dose. With a mask, that number jumps to 89%. That’s why masks are still recommended for kids under six. For older kids, mouthpieces are fine - but only if they seal their lips tightly around it.How to Use a Spacer Correctly (Step by Step)
It sounds simple, but most families get it wrong. Here’s the right way, based on guidelines from the Royal Children’s Hospital and the Allergy & Asthma Network:- Have your child sit upright - no lying down or slouching.
- Attach the inhaler to the spacer. Make sure it’s clicked in securely.
- If your child is under six, put the mask on their face. It needs to cover the nose and mouth with no gaps.
- Shake the inhaler well.
- Press the inhaler once - only one puff at a time.
- Let your child breathe in and out slowly through the spacer four times. Count to five with each breath.
- Wait 30 seconds before giving a second puff, if needed.
- Wash the spacer once a week with warm water and dish soap. Don’t rinse it - just let it air dry. Rinsing creates static that traps medicine.
- Never wipe the inside dry with a towel. Static builds up, and the medicine sticks to the walls.
What Schools Need to Know (and Do)
School is where asthma problems often get worse. Kids are active, exposed to triggers like chalk dust or pollen, and may not have their inhaler handy. That’s why every school with students who have asthma needs a clear plan. The National Asthma Education and Prevention Program says all students with asthma should have an individualized asthma action plan on file. That plan includes:- What triggers make their asthma worse
- Which medications they take and when
- When to use the spacer and inhaler
- When to call 911 or go to the ER

The Teen Problem: Why Older Kids Stop Using Spacers
Here’s the hard truth: kids who use spacers well at age 6 often stop by age 14. Why? Because they feel different. They’re embarrassed. They don’t want to be the kid who pulls out a big plastic tube in front of friends. A 2022 study found adolescents are 80% less likely to use their inhaler correctly than younger children. The spacer is bulky. It doesn’t fit in a jeans pocket. It looks medical. And teens hate standing out. Some manufacturers make smaller, sleeker spacers now - some even come in colors or with cartoon designs. But many schools still only stock the standard white plastic ones. That’s a missed opportunity. The fix isn’t just better devices. It’s better culture. Schools that treat asthma like any other health need - like wearing glasses or having an EpiPen - see better compliance. Teachers who say, “I keep a spacer in my desk for emergencies,” normalize it. When kids see adults using them without shame, they’re more likely to follow.Building a Real Asthma Care Plan
An asthma care plan isn’t a piece of paper. It’s a living tool. Here’s what it needs to include:- Green zone: When the child is doing fine. List daily meds and triggers to avoid.
- Yellow zone: Early warning signs - coughing at night, shortness of breath during play. List what to do: use spacer + inhaler, rest, monitor.
- Red zone: Emergency signs - struggling to breathe, lips turning blue, voice barely a whisper. List: use spacer + inhaler immediately, call 911, go to ER.
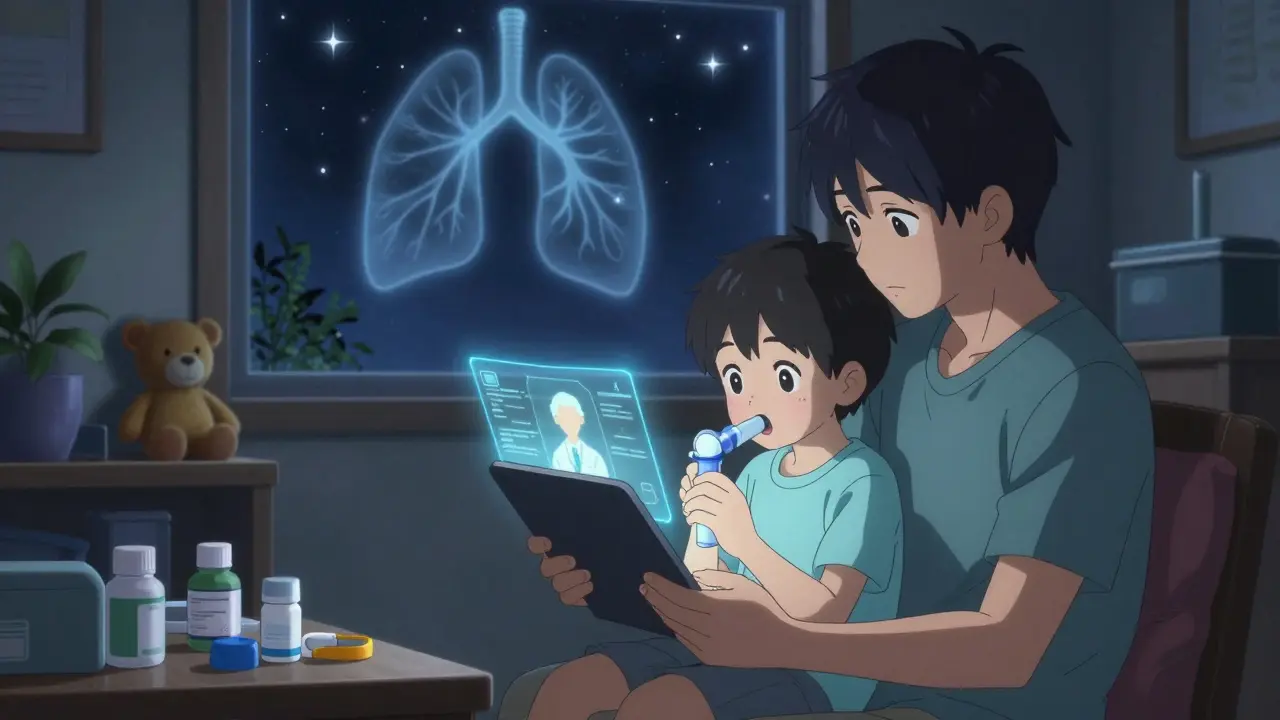
What’s Next? Technology and Better Access
The future of asthma care is getting smarter. The NIH is funding a $2.5 million study to test smartphone apps that track spacer use in school. The idea? A tiny sensor in the spacer sends a notification when it’s used - and reminds the child if they forget. If the app shows they haven’t used it in 24 hours, the school nurse gets an alert. Some new spacers are even designed to be quieter and smaller. One model, tested in 2023, is the size of a lipstick and clips to a keychain. It’s not yet widely available, but it’s a sign of where things are headed. Meanwhile, the CDC’s National Asthma Control Program is now funding spacer distribution in underserved school districts. If your child’s school doesn’t have spacers, ask. You’re not asking for a favor - you’re asking for a basic health safety net.Final Thought: It’s Not About the Device. It’s About the System.
A spacer won’t help if no one knows how to use it. A care plan won’t matter if the school doesn’t have it on file. A child won’t feel safe if they’re ashamed to use their inhaler. The best asthma management isn’t just medical - it’s social. It’s teachers who know what to do. It’s classmates who don’t stare. It’s a spare spacer in the nurse’s office, clean and ready. It’s a parent who checks the plan every season. Asthma doesn’t go away. But with the right tools and support, it doesn’t have to control a child’s life either.Can my child use an inhaler without a spacer?
For children under 12, using an inhaler without a spacer is not recommended. Most kids can’t coordinate pressing the inhaler and breathing in at the same time. Without a spacer, up to 80% of the medicine ends up in the mouth or throat, not the lungs. Spacers make treatment more effective and reduce side effects. Even older kids benefit - studies show teens who use spacers have fewer hospital visits.
How often should I clean my child’s spacer?
Clean the spacer once a week with warm water and a drop of dish soap. Don’t rinse it after washing - just let it air dry. Rinsing creates static, which traps the medicine inside the spacer. Never wipe the inside with a towel or paper towel. That also creates static. If the spacer gets wet from sweat or moisture, don’t use it. Use a spare one instead.
Does my child’s school have to have a spacer available?
In 42 U.S. states, schools are legally required to keep asthma medication - including spacers - on site for students with asthma. Even if your state doesn’t require it, schools receiving federal funding must follow the National Asthma Education and Prevention Program guidelines, which recommend having rescue inhalers and spacers accessible. If your child’s school doesn’t have one, ask for it in writing. You’re not asking for special treatment - you’re asking for a basic safety measure.
My teen refuses to use the spacer at school. What can I do?
Start by talking to your teen about why they’re embarrassed. Many feel like they’re being singled out. Try switching to a smaller, colored spacer or one with a design they like. Talk to the school nurse about letting your teen keep the spacer in their locker or backpack instead of carrying it visibly. Ask if the school can train staff to quietly assist during an attack - so your child doesn’t have to draw attention. Normalizing asthma care helps. If teachers and nurses treat it like checking blood sugar or wearing glasses, your teen will feel less alone.
What’s the difference between a spacer and a nebulizer?
A nebulizer turns liquid medicine into a mist you breathe through a mask or mouthpiece. It takes 10-15 minutes and needs electricity. A spacer is a plastic tube that attaches to a handheld inhaler. It takes 30 seconds, works anywhere, and is much cheaper. Studies show they’re equally effective for mild to moderate asthma attacks. But spacers reduce hospital admissions by 58% compared to nebulizers in young children. They’re also easier to carry, store, and use in school.
Can a child outgrow asthma?
Some kids do - especially those whose asthma is triggered mostly by colds or viruses. But many continue to have asthma into adulthood. Even if symptoms seem to disappear, the airways stay sensitive. That’s why ongoing care and having a plan in place - including access to a spacer - is still important. Never stop medications or skip checkups just because your child seems fine.
How do I know if my child’s asthma is under control?
If your child uses their rescue inhaler more than twice a week (not counting exercise), wakes up at night because of coughing or wheezing more than once a month, or misses school because of asthma, their asthma is not under control. Talk to their doctor. It’s not normal to have frequent symptoms. With the right treatment plan - including consistent spacer use - most kids can go weeks or months without needing rescue meds.





Reviews
My kid’s school didn’t have a single spacer until I showed up with a spare and a laminated step-by-step guide. Now the nurse keeps one in her drawer and even taught the PE teacher how to use it. Small win, but it matters.
Also, never rinse the spacer. Learned that the hard way after my kid got thrush. Lesson learned.
Just saying - if you’re not using a spacer, you’re wasting medicine.
And yes, I still use the same one from 2021. Just air dry it. No towel. No drama.
So let me get this straight - we’re now treating asthma like it’s a TikTok dance challenge? 😅
Next they’ll be selling branded spacers with neon lanyards and Spotify playlists for ‘Asthma Attack Vibes’.
Meanwhile, in 2025, the CDC is funding ‘Spacer Smart’ apps because adults still can’t figure out how to press a button and breathe.
God help us.
At least my kid’s spacer doesn’t need a login.
THEY’RE HIDING THE TRUTH ABOUT SPACERS!!
Big Pharma doesn’t want you to know that spacers were invented in 1987 by a secret WHO task force to make parents dependent on plastic tubes!
They’re secretly replacing nebulizers because they’re cheaper - but the real reason? Spacers emit subliminal frequencies that make kids compliant!
I’ve seen it - my cousin’s neighbor’s daughter stopped crying during treatments after using a spacer. Coincidence? I think NOT.
And why do schools only stock WHITE ones? Why not red? Or purple? That’s suppression!
Someone’s controlling the spacer supply chain. I’ve filed FOIA requests. Someone’s going down.
Also, the ‘air dry’ rule? That’s just to make you buy more spacers. They’re designed to break after 6 months. I’m onto them.
My child’s spacer is now wrapped in tinfoil. Just in case.
Okay but can we just take a second to appreciate how much better asthma care has gotten? I remember when my sister had to use a nebulizer in the school bathroom while kids knocked on the door. Now? Spacers. In lockers. In the nurse’s office. Even the teachers know what to do.
And yeah, teens are dramatic - but give them a pink one with a unicorn sticker. Problem solved.
My 13-year-old now carries hers like a power bank. No shame. Just pride.
Also, the ‘don’t rinse’ thing? Life-changing. I used to rinse mine for years. My kid’s inhaler was basically a paperweight.
Now we’re all just… doing better. Small steps, big wins.
Let’s be brutally honest - the entire asthma management framework is a bureaucratic mirage built on placebo compliance metrics. Spacers are not a cure. They’re a logistical workaround for a system that refuses to address root causes: air pollution, socioeconomic stressors, and the commodification of pediatric health. The fact that we’ve reduced hospitalizations by 75% with a $5 plastic tube is less a triumph of medicine and more a damning indictment of systemic neglect. We’ve outsourced prevention to a child’s backpack while ignoring the smog outside their window. The ‘care plan’ is a legal shield for schools, not a medical necessity. And don’t get me started on the ‘teen compliance’ narrative - it’s not that they’re embarrassed, it’s that they’re rational. Why should a 14-year-old submit to a ritual designed for toddlers? The spacer is a relic of pediatric paternalism. The real innovation would be inhalers with built-in dose sensors and AI-triggered alerts - not more plastic tubes and laminated posters. We’re treating symptoms while the infrastructure crumbles. This isn’t progress. It’s damage control dressed in green zones.
42 states require spacers? That’s pathetic. In my state, we don’t even let kids bring inhalers to school unless they’ve got a notarized affidavit signed by the mayor and the Pope. This is America - we don’t need plastic tubes. We need discipline. My son had asthma and I made him breathe through a straw for 10 minutes every day. Toughened him up. Now he runs track. No spacer. No problem.
Also, why are we letting schools handle this? It’s the parents’ job. You want your kid to breathe? Don’t let them get fat. Don’t let them play outside. Stop using scented candles. Simple.
Spacers? That’s a crutch. Real Americans don’t need gadgets. We need grit.
Okay but have you seen the new FluxAir spacer? 🤯 It’s the size of a Bic pen, charges via USB-C, and syncs with Apple Health. My kid’s school just rolled them out - and yes, it’s available in matte black, rose gold, and ‘Asthma Warrior’ glow-in-the-dark.
Meanwhile, in the U.S., schools are still using 2012-era white tubes that look like they were salvaged from a 90s science fair.
Canada’s been doing this since 2018. We even have spacer vending machines in high schools. You scan your student ID, get a fresh one, and the system logs usage. No static. No drama. Just efficiency.
Why are we still pretending this is 2005? 🤦♂️
I just wanted to say thank you for writing this. My daughter started using a spacer last year and now she’s back on the soccer team. We didn’t even know how to use it right until the school nurse showed us. It’s not about the device - it’s about having someone who cares enough to show you how.
Also, air dry. Not rinse. I’m telling you, that one tip saved us from three ER trips.
Small things, big difference.
My kid’s school didn’t have a spacer until I brought one in. Now they keep two. One in the office, one in the bus. Cleaned weekly. Air dried. No towel. No rinse. Simple.
Also - teens are weird. They’ll use it if it’s not obvious. Got him a black one. Keeps it in his hoodie. No one notices.
Good post. Just needed to say it.