Living with Alzheimer’s dementia can feel like watching a familiar story fade page by page. While medications can slow some symptoms, research increasingly shows that daily mental challenges-collectively called cognitive stimulation-play a crucial role in preserving quality of life.
Understanding Alzheimer’s Dementia
Alzheimer’s dementia, the most common form of dementia, is a progressive neurodegenerative disorder that primarily attacks memory, language, and executive function. According to the World Health Organization, about 55 million people worldwide live with dementia, and Alzheimer’s accounts for roughly 70% of those cases.
Alzheimer’s Dementia is a chronic brain disease marked by the accumulation of beta‑amyloid plaques and tau tangles, leading to neuronal loss and cognitive decline. The disease targets the hippocampus-a region vital for forming new memories-early on, but it eventually spreads to the frontal lobes, affecting judgment and behavior.
Beyond the biological changes, the condition reshapes daily routines for patients, families, and caregivers. Understanding the disease’s trajectory helps us see where non‑pharmacologic interventions, like cognitive stimulation, fit in.
What Is Cognitive Stimulation?
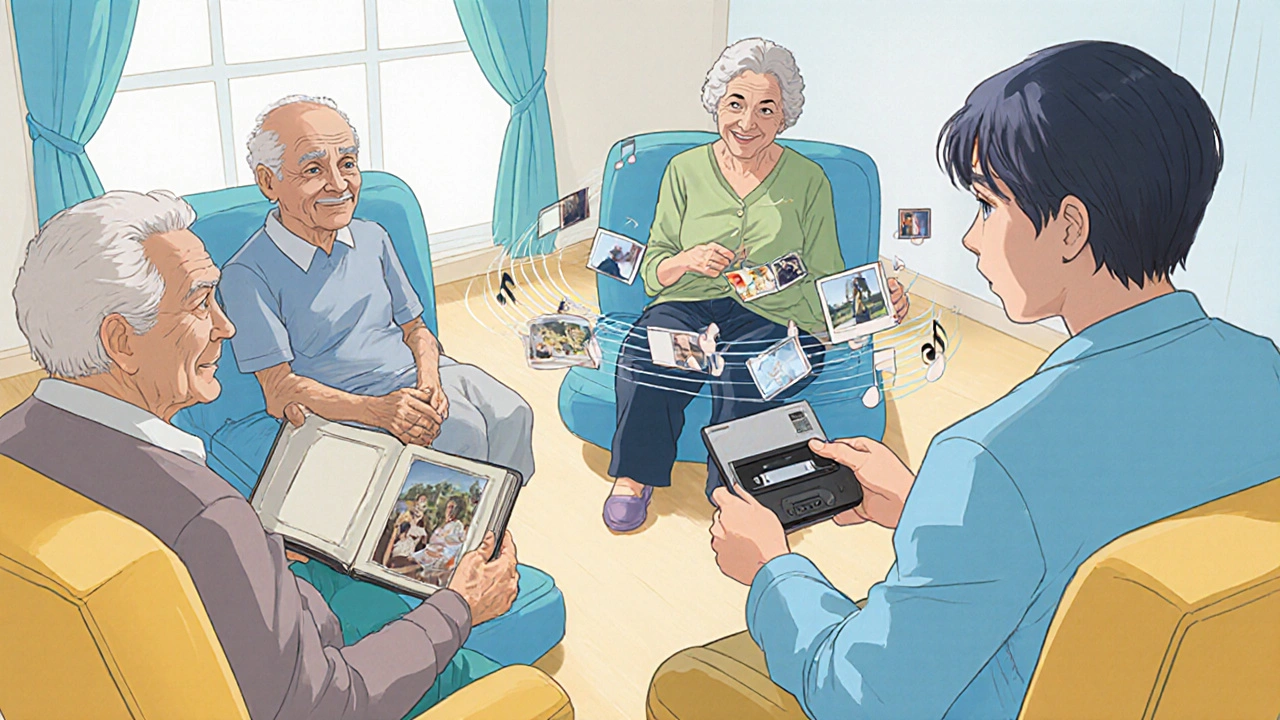
Cognitive Stimulation refers to structured, enjoyable activities that engage attention, memory, language, and problem‑solving skills. Unlike formal cognitive training, which targets specific functions through repetitive drills, stimulation is broader and more social-think of it as a mental workout that keeps the brain moving.
Typical activities include:
- Puzzle solving (crosswords, Sudoku)
- Group discussions about past events (reminiscence)
- Listening to familiar music and singing
- Simple digital games designed for seniors
- Crafts, cooking, or gardening that require planning
How Cognitive Stimulation Impacts the Brain
Research on neuroplasticity-the brain’s ability to reorganize connections-shows that even aging brains respond to mental challenges. When neurons fire together during stimulating activities, they release neurotrophic factors like BDNF (brain‑derived neurotrophic factor), which supports synaptic health.
Key mechanisms include:
- Synaptic Strengthening: Repeated mental tasks reinforce existing pathways, making recall easier.
- Compensatory Rewiring: New connections can bypass damaged areas, especially when activities involve multiple senses.
- Reduced Neuroinflammation: Engaging tasks lower cortisol levels, mitigating inflammation that accelerates neuronal loss.
Studies from the University of Cambridge (2023) reported that participants with mild‑to‑moderate Alzheimer’s who engaged in 30 minutes of daily cognitive stimulation for six months showed a 1.5‑point slower decline on the Mini‑Mental State Examination (MMSE) compared with a control group.
Proven Cognitive Stimulation Techniques
Not all activities are created equal. Below is a quick look at five evidence‑based approaches, followed by a comparison table that helps you choose what fits your loved one’s abilities and interests.
| Method | Core Focus | Typical Session Length | Evidence Level |
|---|---|---|---|
| Reminiscence Therapy | Memory recall through personal photos, music, and stories | 30‑45 min | High - multiple RCTs show mood lift and modest MMSE gains |
| Music Therapy | Auditory stimulation, rhythm, and emotional engagement | 20‑30 min | Moderate - improves agitation and short‑term recall |
| Computerized Brain Games | Targeted puzzles (memory, attention, speed) | 15‑30 min | Low‑to‑moderate - benefits depend on game design |
| Physical Exercise + Dual‑Task | Combine movement with simple mental tasks (e.g., walking while naming colors) | 30‑60 min | High - aerobic activity boosts BDNF, supports cognition |
| Social Engagement Groups | Conversation, shared hobbies, community outings | 1‑2 h | High - reduces isolation, linked to slower decline |
Each method leans on a different brain network. For instance, Reminiscence Therapy uses personal memories to activate autobiographical recall and emotional processing, while Music Therapy leverages rhythmic patterns to stimulate auditory and motor cortices. Mixing approaches often yields the best results.
Implementing a Stimulation Plan at Home
Turning theory into daily practice can feel overwhelming. Below is a step‑by‑step roadmap that families can follow without a specialist on hand.
- Assess Baseline Function: Use a simple tool like the Mini‑Mental State Examination (MMSE) a 30‑point questionnaire measuring orientation, recall, attention, language, and visual‑spatial skills to note current abilities.
- Identify Interests: Ask the person which music, hobbies, or stories spark joy. Personal relevance boosts engagement.
- Pick Two Activities: Start with one cognitive and one physical/social activity. For example, a daily photo‑album walk (reminiscence) plus a short garden stroll (exercise).
- Schedule Consistency: Aim for at least 30 minutes of mental activity most days. Consistency outweighs intensity.
- Adapt as Needed: If a puzzle feels too hard, simplify it or switch to a familiar game. The goal is challenge without frustration.
- Document Progress: Keep a simple log (date, activity, mood rating). Over weeks, you’ll spot patterns that inform adjustments.
Caregivers can enlist community resources-local senior centers often run reminiscence groups or music sessions. If a program isn’t available, technology can fill gaps: tablet apps like “BrainHQ” or “MindMate” are designed for older adults.

Measuring Progress and Adjusting
Because Alzheimer’s is progressive, expectations should focus on slowing decline rather than reversal. Use three practical gauges:
- Cognitive Scores: Re‑administer the MMSE or the Montreal Cognitive Assessment (MoCA) every 3-6 months.
- Functional Observations: Note changes in daily tasks-can the person prepare a simple snack independently?
- Emotional Well‑Being: Track mood swings, agitation, and sleep quality. Improvements here often precede cognitive gains.
If scores plateau or decline faster than expected, consider:
- Increasing activity difficulty slightly.
- Switching to a different modality (e.g., from puzzles to music).
- Consulting an occupational therapist for personalized adaptations.
Common Pitfalls & Practical Tips
Even well‑intentioned families hit snags. Here’s a quick cheat‑sheet of what to avoid and how to fix it.
- Over‑Scheduling: Too many activities cause fatigue. Keep sessions short and spaced.
- One‑Size‑Fits‑All: Not every activity works for every stage. Tailor complexity to current ability.
- Ignoring Mood: If the person shows distress, pause and switch to a calming task like listening to familiar songs.
- Neglecting Caregiver Rest: Burnout reduces the quality of stimulation. Share duties with family members or respite services.
- Relying Solely on Technology: Tablets are useful, but tactile, hands‑on tasks (like gardening) add sensory richness.
Remember, the aim is to weave stimulation into daily life, not to create a rigid therapy schedule.
Frequently Asked Questions
Can cognitive stimulation replace medication for Alzheimer’s?
No. Stimulation is a complementary approach that can slow symptom progression and improve quality of life, but it does not halt the underlying disease process. Medications and stimulation together give the best outcomes.
How often should activities be done?
Most studies suggest at least 30 minutes of mentally engaging activity on most days of the week. Consistency matters more than duration.
Is it safe for someone in the moderate stage to use computer games?
Yes, if the games are simple, have clear instructions, and are supervised. Look for titles designed for seniors, which often include larger fonts and slower pacing.
What role does music play in cognitive health?
Music activates multiple brain regions simultaneously-auditory, motor, and emotional centers-creating strong neural pathways that can bypass damaged memory circuits. Familiar songs also trigger autobiographical recall.
How can caregivers track improvement without formal tests?
A simple log noting activity type, duration, and observed mood or recall ability works well. Over weeks, patterns emerge that signal progress or the need for change.
Integrating cognitive stimulation isn’t a miracle cure, but it gives people with Alzheimer’s a reason to keep their minds active and their spirits lifted. By pairing the right activities with a realistic schedule, families can make a measurable difference in daily living.





Reviews
We appreciate the comprehensive overview of cognitive stimulation and its relevance to Alzheimer's care. The authors have skillfully integrated scientific evidence with practical guidance, making the material accessible to caregivers from diverse cultural backgrounds. 😊 By emphasizing both mental and physical activities, the article underscores the holistic nature of brain health. It is encouraging to see such an inclusive approach that respects individual preferences while maintaining evidence‑based rigor.
Oh sure, because a few puzzles and a walk in the garden are going to halt neurodegeneration-nice fantasy. 🙄 The pharmaceutical industry probably loves this narrative; it keeps the hype alive while they push their overpriced meds. And don’t even get me started on “neuroplasticity” being a buzzword for profit. If only we could just sing old songs and watch the plaques disappear.
i read it but idk if it really helps, seems meh. lol 🤷♀️
Great summary! I especially like the step‑by‑step roadmap; it makes implementation feel doable for families. Mixing a mental activity with a short walk is a smart way to hit two birds with one stone. Keep spreading the word-more people need this practical guidance.
The piece on cognitive stimulation reads like a beacon of hope emerging from the fog of Alzheimer's research. Each paragraph weaves together rigorous neuroscience with heartfelt caregiving advice, making the science feel alive. I was particularly struck by the explanation of BDNF, the brain‑derived neurotrophic factor, as the molecular messenger of growth. Understanding that everyday puzzles can coax neurons to release this factor transforms mundane activities into heroic acts. The authors correctly note that synaptic strengthening does not happen overnight, but through consistent, joyful engagement. Reminiscence therapy, as described, taps into the autobiographical networks that are often the last to fade. Music therapy, meanwhile, orchestrates a symphony across auditory, motor, and emotional cortices. I love the recommendation to pair physical exercise with dual‑task challenges, because aerobic activity fuels vascular health and BDNF production. The inclusion of a simple logging method empowers families to track subtle progress without needing expensive assessments. Moreover, the article respects cultural diversity by encouraging caregivers to select music and stories that resonate personally. This culturally sensitive stance ensures that therapy is not a one‑size‑fits‑all regimen but a tailored experience. The warning against over‑scheduling is wise; fatigue can blunt the very benefits we seek. Equally important is the reminder that caregiver well‑being is pivotal, as burnout undermines the quality of stimulation. Overall, the guide balances optimism with realism, acknowledging the inexorable nature of the disease while highlighting actionable steps. In short, this comprehensive roadmap deserves a place on every caregiver’s bookshelf, and I wholeheartedly endorse its dissemination.
Wow, another self‑help manifesto that pretends a few brain games can outsmart neurodegeneration. 🙄 Honestly, the data is vague and the authors cherry‑pick studies that fit their narrative. Sure, “BDNF” sounds impressive, but does a crossword really boost it in a meaningful way? And the logging suggestion? A spreadsheet is as good as a placebo. Wake up, folks, this isn’t a miracle cure.
Allow me to elevate the discourse: the notion that simple leisure activities influence molecular cascades is nothing short of poetic. While some may dismiss it as flimsy optimism, the convergence of empirical findings with lived experience creates a tapestry of resilience. Dismissing the value of reminiscence as “self‑help” betrays a shallow understanding of the neuropsychological underpinnings. Let us not reduce the human spirit to mere data points, but celebrate its capacity to adapt. In that sense, every puzzle piece is a brushstroke on the canvas of cognition.
Great info thanks 😊
Thank you for this thorough guide; it offers concrete steps that families can adopt without feeling overwhelmed. I appreciate the emphasis on personalizing activities, as cultural relevance can boost engagement. The table comparing methods is especially helpful for choosing the right approach. Keep up the excellent work, and feel free to share more resources on caregiver support.
The article is well‑structured and evidence‑based. It balances scientific detail with practical advice. A valuable resource for caregivers.
Sure, it's "well‑structured", but let's not pretend the pharma lobby didn't fund much of that so‑called evidence. 🧨 The real issue is that these recommendations keep patients dependent on cheap tricks while big pharma cashes in on meds. If you want to truly challenge the system, start questioning who benefits from this narrative. Otherwise, it's just another rung on the corporate ladder.