When your big toe suddenly swells up so badly you can’t even wear a sock, and the pain feels like your joint is on fire, you’re not just having a bad day-you’re having a gout attack. This isn’t just ‘bad arthritis.’ It’s a specific, intense inflammatory reaction caused by tiny, sharp crystals of uric acid building up in your joints. And if you’ve had one, you know: it doesn’t just go away on its own. You need to understand what’s happening inside your body, what’s triggering it, and how to stop it from coming back.
What Exactly Is Uric Acid Doing in Your Joints?
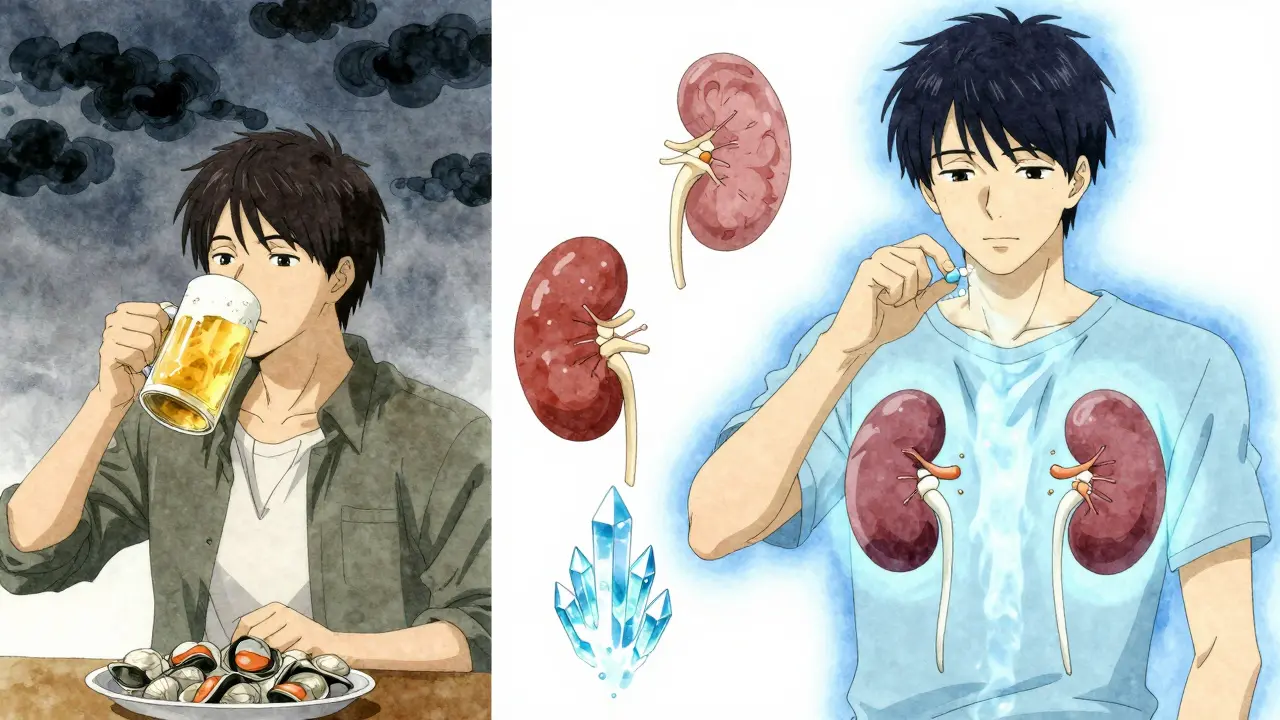
Uric acid is a waste product your body makes when it breaks down purines-natural substances found in your cells and in certain foods. Most people’s kidneys flush it out without issue. But in gout, something goes wrong. Either your kidneys aren’t clearing it well enough, or your body is making too much. Either way, the level in your blood climbs above 6.8 mg/dL. That’s the saturation point. Once it hits that number, uric acid starts forming hard, needle-like crystals in and around your joints.These crystals don’t just sit there quietly. They trigger your immune system like an alarm. Special immune cells called macrophages see them as invaders and activate something called the NLRP3 inflammasome. That sets off a chain reaction, releasing a powerful inflammatory signal called interleukin-1β. That’s what causes the redness, heat, swelling, and pain-sometimes so severe it wakes you up at night.
What makes gout uniquely human? Most animals have an enzyme called uricase that breaks down uric acid into something harmless. Humans lost that gene during evolution. So we’re stuck with higher levels, making us more vulnerable. About 90% of gout cases happen because the kidneys aren’t excreting enough uric acid-not because you’re eating too much meat. Genetics play a huge role here. Variants in genes like SLC2A9 and ABCG2 can make your kidneys reabsorb more uric acid than they should, pushing levels up even if your diet is fine.
What Triggers a Gout Attack? It’s Not Just Beer
Many people think gout flares are caused by eating too many steaks or drinking too much beer. That’s part of it, but it’s more complex. A flare doesn’t happen just because uric acid is high-it happens when something causes a sudden change in crystal stability.Here are the real triggers:
- Dehydration: When you don’t drink enough water, your urine output drops below 1.5 liters a day. That means uric acid concentrates in your blood and joints, making crystals more likely to form or break loose. This is especially common after alcohol, intense exercise, or illness.
- Rapid changes in uric acid levels: This is the most overlooked trigger. Starting or changing urate-lowering medication like allopurinol can cause a flare-even though the drug is meant to help. Why? Because any big shift in uric acid concentration, up or down, can destabilize crystals in your joints. That’s why doctors now recommend starting anti-inflammatory drugs like low-dose colchicine when you begin treatment.
- Joint trauma: Even a minor injury, like stubbing your toe or wearing tight shoes, can physically disrupt crystals in the joint, triggering inflammation.
- Alcohol: Beer is the worst offender. A 12-ounce serving increases your risk of a gout attack by 49%. Why? Beer is high in purines and also slows down how fast your kidneys clear uric acid. Spirits are less risky, but still raise your risk by 15%. Wine has the least effect.
- Fructose: Sugary drinks-soda, sweetened iced tea, energy drinks-are a hidden culprit. Fructose boosts uric acid production by 20-30% because it breaks down in the liver and depletes ATP, which then turns into purines.
- High-purine foods: Organ meats (liver, kidney), shellfish (shrimp, mussels), and certain fish (anchovies, sardines) pack in 300-500 mg of purines per 3-ounce serving. Red meat is less intense but still contributes. Poultry and most vegetables? Not a problem.
Here’s the twist: dairy doesn’t just avoid triggering gout-it helps prevent it. Low-fat milk and yogurt reduce your risk by 43% per daily serving. The proteins in milk seem to help your kidneys excrete more uric acid.
How Do You Treat a Gout Attack Right Now?
When the pain hits, you need fast relief. But not all painkillers work the same. You can’t just pop ibuprofen and call it done.Doctors have three main first-line options for acute flares:
- NSAIDs: Indomethacin (50 mg three times a day) is the classic choice. Naproxen or celecoxib are alternatives. They reduce inflammation quickly but can irritate your stomach or hurt your kidneys if you’re already at risk.
- Colchicine: Taken at 0.6 mg three times a day for the first day, then cut back to once or twice daily. It blocks the immune response to crystals. Side effects? Diarrhea-about 1 in 5 people get it. Lower doses work just as well with fewer stomach issues.
- Corticosteroids: If you can’t take NSAIDs or colchicine, a short course of prednisone (30-40 mg daily for 5 days, then tapered) works just as well. It’s especially useful if you have kidney problems or stomach ulcers.
Important: Don’t start or stop any of these drugs during a flare unless your doctor tells you to. And never take aspirin-it blocks uric acid clearance and makes flares worse.
Long-Term Strategy: Lowering Uric Acid for Good
Treating the pain is only half the battle. If you don’t lower your uric acid levels over time, you’ll keep having flares. And over years, those crystals turn into hard lumps called tophi-visible under the skin, damaging joints, and sometimes breaking through the skin.The goal? Keep your serum uric acid below 6 mg/dL. For people with tophi or frequent flares, aim for 5 mg/dL or lower. Studies show that if you hit that target for a full year, 70% of tophi disappear.
Here’s how doctors get you there:
- Allopurinol: First-line treatment. Starts at 100 mg daily. Your doctor will increase the dose by 100 mg every 2-5 weeks until your uric acid is in target range. Most people need 300-600 mg daily. Some need up to 800 mg. It’s safe, cheap, and works for almost everyone-even those with kidney disease.
- Febuxostat: Used if you can’t tolerate allopurinol. Takes 40-80 mg daily. Works similarly but is more expensive. Not recommended if you have heart disease.
- Probenecid: A uricosuric drug that helps your kidneys flush out more uric acid. Only works if your kidneys are healthy (GFR above 50 mL/min). Not for people with kidney stones.
Here’s the critical part: you must take these medications every day, even when you feel fine. If you stop, your uric acid levels bounce back in 2-4 weeks, and flares return. Many patients stop allopurinol during a flare, thinking it’s causing the pain. That’s backwards. The flare is caused by changing levels-not the drug itself.
Prophylaxis: Preventing Flares When You Start Treatment
Starting allopurinol or febuxostat is like shaking a snow globe. The crystals move. That’s why 30-40% of people get flares in the first six months of treatment.The solution? Anti-inflammatory prophylaxis. The American College of Rheumatology recommends low-dose colchicine (0.6 mg once or twice daily) for at least six months after starting urate-lowering therapy. Studies show this cuts flare risk by 50-75% compared to no prevention.
If you can’t take colchicine, low-dose NSAIDs or even low-dose prednisone can be used. But don’t skip this step. It’s not optional-it’s essential to long-term success.

Diet and Lifestyle: What Actually Works
You don’t need to become a vegan to control gout. But you do need to make smart, consistent changes:- Hydrate: Drink at least 2 liters of water a day. More if you’re active or in hot weather. Water helps your kidneys flush uric acid.
- Choose low-fat dairy: One or two servings a day lowers your risk. Skim milk, cottage cheese, yogurt.
- Avoid sugary drinks: No soda, no energy drinks, no sweetened juices. Switch to water, tea, or coffee (coffee may even help lower uric acid).
- Limit alcohol: If you drink, stick to wine. Keep beer under one 12-ounce serving per day. Avoid binge drinking.
- Reduce high-purine foods: Skip organ meats, shellfish, and anchovies. You can still eat chicken, turkey, and most vegetables. Lentils and beans? Fine.
- Maintain a healthy weight: Losing even 5-10% of body weight can lower uric acid by 1-2 mg/dL.
There’s no magic food that cures gout. But consistent habits make a huge difference.
What About New Treatments?
The future of gout treatment is getting exciting. Researchers are now targeting the inflammation itself-not just uric acid.Drugs like dapansutrile, which block the NLRP3 inflammasome, are in phase III trials. Early results show they cut flare duration by 40% compared to placebo. That’s the first treatment designed to stop the immune response at its source.
Another area? Gut health. Early studies suggest certain probiotics may help your body break down purines more efficiently, lowering uric acid by 10-15%. It’s not a replacement for medication yet-but it’s a promising add-on.
Monitoring and Long-Term Care
Gout isn’t something you treat once and forget. It’s a chronic condition that needs lifelong management.- Check your uric acid level every 2-5 weeks when adjusting medication.
- Once you’re stable, check every 6 months.
- Get imaging (ultrasound or dual-energy CT) if you have tophi or frequent flares. It shows crystal buildup even when you’re not in pain.
- Never stop your urate-lowering drug without talking to your doctor.
And here’s the most important thing: gout isn’t cured when the pain stops. It’s controlled when your uric acid stays low. If you think you’re fine after one flare, you’re setting yourself up for more pain down the road.
Can gout be cured with diet alone?
No. While diet helps reduce flare frequency and lowers uric acid slightly, it’s rarely enough to get levels below 6 mg/dL on its own. Most people need medication to reach and maintain the target level. Diet is a support tool, not a cure.
Why does my gout flare up even when I’m not eating trigger foods?
Gout flares are triggered by changes in uric acid levels-not just high levels. Dehydration, stress, sudden weight loss, starting or changing medication, or even minor joint trauma can destabilize crystals and cause a flare-even if your diet has been perfect.
Is it safe to take allopurinol if I have kidney disease?
Yes. Allopurinol is safe for people with kidney disease and is actually preferred over other urate-lowering drugs in this group. Your doctor will adjust the dose based on your kidney function, but it’s still the most effective long-term option.
How long until tophi disappear?
If you keep your serum uric acid below 5 mg/dL for 12 months, about 70% of tophi shrink or disappear completely. It takes time-often 1-2 years-because crystals dissolve slowly from deep in the joints and tissues.
Can I drink alcohol if I have gout?
You can, but you must be strict. Beer is the worst-it increases flare risk by nearly 50% per daily serving. Spirits raise risk by about 15%. Wine has the least effect. If you drink, limit beer to one 12-ounce serving per day, and avoid binge drinking. Many people do better by cutting it out entirely.
If you’ve had more than two gout attacks in a year, or if you see lumps under your skin, talk to your doctor about starting long-term urate-lowering therapy. Don’t wait for the next flare. The goal isn’t just pain relief-it’s preventing permanent joint damage and getting your life back.






Reviews
Man I thought I was the only one who got nailed by gout after a night of whiskey and pizza 🤯
Turns out it’s not just the beer - dehydration and sudden uric acid shifts are the real killers
I started drinking 3L of water a day and now I’m down to one flare a year instead of monthly
Also low-fat yogurt is my new best friend 😌
Stop blaming your diet. You think this is about what you eat? No. It’s about your kidneys being lazy and your genes being broken. I’ve seen people eat tofu and kale and still have tophi. The system is rigged.
Allopurinol isn’t a cure - it’s a Band-Aid on a leaking dam.
Let me tell you something I learned the hard way after five years of gout flares and three ER visits
You don’t need to give up everything to control this
Hydration is the silent hero - I drink a liter before bed and another first thing in the morning
Low-fat dairy every day - I put it in my coffee and it’s been a game changer
And yes I still eat chicken and beans - turns out they’re fine
But I stopped drinking soda cold turkey and my uric acid dropped 2 points in six weeks
The real secret? Consistency. Not perfection. Just showing up every day with water, milk, and zero sugar drinks
And if you’re on allopurinol - don’t quit when you flare. That’s like stopping your blood pressure med when your head hurts.
It’s not the drug causing it - it’s your body adjusting
And yes, I know people say it’s all about diet - but genetics and kidney function matter way more than you think
Don’t let anyone make you feel guilty for eating steak once a month
You’re not failing - you’re managing a chronic condition
And if you’re not on prophylaxis when starting meds - you’re doing it wrong
Colchicine isn’t optional - it’s your body’s seatbelt during the uric acid crash
Y’all are overcomplicating this. Beer = bad. Sugar = worse. Stop drinking and you’ll be fine. No magic. No science. Just stop being lazy.
My uncle had tophi for 15 years and quit alcohol and soda - poof. Gone. No meds. No drama.
Stop blaming your genes. You’re just weak.
Correction: The article states that 90% of gout cases are due to renal underexcretion - but this is misleading without context. The original 1998 study cited only included patients with hyperuricemia, not the general population. Also, the claim that 'wine has the least effect' is contradicted by a 2020 meta-analysis in Arthritis & Rheumatology showing moderate wine intake increases risk by 11% - not negligible. And no, coffee doesn't 'lower uric acid' - it mildly inhibits xanthine oxidase, but the effect is clinically insignificant in most. Also, 'low-fat dairy reduces risk by 43%' - that’s relative risk, not absolute. Your baseline risk is 0.5%. So 43% reduction = 0.7%. Not a miracle.
Don’t let anecdotes masquerade as evidence.
They don’t want you to know this but the FDA and Big Pharma are hiding the real cause - EMF radiation from your phone and wifi routers is breaking down your purines into uric acid faster. That’s why it’s getting worse every year. And they’re pushing allopurinol because it’s profitable. The truth? Your gut microbiome is poisoned by glyphosate in your food. Take probiotics - real ones, not the junk in the store. I took 12 strains for 3 months and my flares stopped. No meds. No doctors. Just truth.
Ugh I’m so tired of this gout stuff. Can’t we just all agree that it’s just old people being dramatic? I mean, I had a toe flare once and it was annoying but like… get over it. Why does everyone make it sound like a death sentence? It’s not cancer. Stop being so sensitive.
Wow. Just… wow. You people think this is just about uric acid? You’re missing the bigger picture. This isn’t a medical condition - it’s a spiritual wake-up call. Your body is screaming that you’ve been living out of alignment. Sugar, stress, and denial - that’s the real toxin. I healed my gout with crystals, breathwork, and cutting out dairy. No meds. No science. Just soul work. If you’re still on allopurinol, you’re not ready to heal. You’re still in fear.