Inflammation Lifestyle Calculator
This calculator estimates how your lifestyle choices may be affecting inflammation levels in Multiple Sclerosis. Based on evidence from the article, lifestyle modifications can help manage inflammation. Enter your current habits to see how they might influence your inflammatory state.
Your Inflammation Score
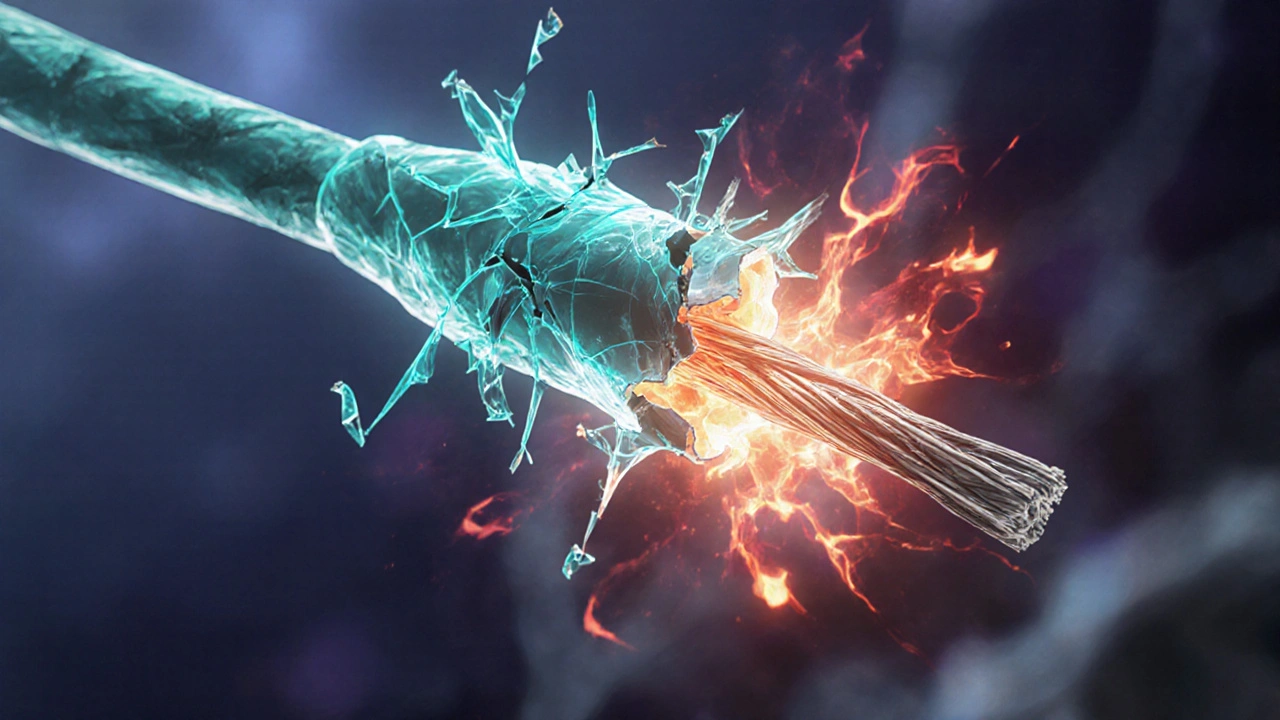
Imagine your nerves are like insulated wires. When the insulation strips away, the signal gets fuzzy, and the whole system suffers. That’s essentially what happens in Multiple Sclerosis is a chronic autoimmune disease that attacks the central nervous system, leading to loss of myelin and neurological disability. The hidden culprit behind this insulation loss is inflammation is the body's natural immune response to injury or infection, characterized by swelling, heat, pain, and cellular activity. Understanding how that immune fire fuels MS can help patients, families, and clinicians spot early signs, choose smarter treatments, and even tweak daily habits to keep the blaze under control.
What triggers inflammation in the first place?
Inflammation starts when the immune system is a complex network of cells, tissues, and organs that defends the body against pathogens and abnormal cells spots something it thinks is dangerous. In MS, the danger isn’t an outside invader but the body’s own myelin and the cells that produce it. The immune system mistakenly flags these elements as foreign, launching an attack that brings a flood of immune cells into the brain and spinal cord.
The key players: T cells, B cells, and microglia
Two types of white blood cells dominate the early assault: T cells are lymphocytes that recognize specific antigens and coordinate immune responses and B cells produce antibodies that target antigens and can present them to T cells. When they cross the blood‑brain barrier, they release enzymes and reactive oxygen species that chew away myelin.
Resident immune cells called microglia are the brain's innate immune cells that survey and respond to injury also join the party. They become activated, sprouting arms that release inflammatory molecules and further damage the surrounding tissue.
When cytokines go rogue
The messengers that amplify the attack are cytokines-tiny proteins that tell other cells what to do. In MS lesions, a handful of cytokines show up in high concentrations, turning a local flare into a full‑blown fire. Below is a quick look at the most notorious ones.
| Marker | Primary Source Cell | Effect on CNS |
|---|---|---|
| Interleukin‑6 (IL‑6) | T cells, astrocytes | Promotes B‑cell activation and blood‑brain barrier permeability |
| Tumor Necrosis Factor‑α (TNF‑α) | Microglia, macrophages | Induces oligodendrocyte death and axonal loss |
| Interferon‑γ (IFN‑γ) | Th1 T cells | Enhances antigen presentation and inflammatory recruitment |
| Interleukin‑17 (IL‑17) | Th17 T cells | Disrupts blood‑brain barrier and attracts neutrophils |
| Granulocyte‑Macrophage Colony‑Stimulating Factor (GM‑CSF) | Th1/Th17 cells | Activates microglia and perpetuates chronic inflammation |
These cytokines don’t act alone; they create feedback loops that keep the immune squad on high alert, even when the initial trigger fades.
Blood‑brain barrier breakdown: the gateway to trouble
The blood‑brain barrier is a selective, tightly‑joined endothelial wall that protects the brain from harmful substances and immune cells normally keeps immune traffic out. In MS, inflammatory cytokines like IL‑6 and TNF‑α loosen the tight junctions, allowing T cells and antibodies to slip through. Once inside, they set up “lesions” that appear as bright spots on MRI scans.

From demyelination to neurodegeneration
At the heart of the damage are oligodendrocytes are the cells that produce myelin sheaths around nerve fibers in the central nervous system. Inflammatory assaults kill or impair these cells, stripping nerves of their protective coating-a process called demyelination is the loss or damage of myelin surrounding nerve fibers, leading to impaired signal conduction. Without myelin, signals slow down or get lost, producing the classic MS symptoms: vision blur, muscle weakness, and coordination problems.
But the story doesn’t stop at myelin loss. Chronic inflammation also harms the underlying axons themselves, a stage known as neurodegeneration. As axons degenerate, the damage becomes permanent, and disability progresses even if active lesions calm down.
Why some people have relapses while others see steady decline
MS comes in different flavors. In the relapsing‑remitting form, inflammatory spikes cause sudden symptom flare‑ups that later improve. In progressive forms, the inflammation becomes low‑grade yet relentless, pushing neurodegeneration forward. Understanding whether the dominant force is acute inflammation or chronic smoldering helps doctors choose the right treatment strategy.
Lifestyle moves that can tip the inflammatory balance
While medication is essential, everyday habits can soften the inflammatory fire. Here are four evidence‑backed actions:
- Vitamin D: Low levels correlate with higher relapse rates; a daily 1000‑2000 IU dose can help maintain immune regulation.
- Omega‑3 fatty acids: Found in fatty fish and flaxseed, they dampen cytokine production and may reduce new lesion formation.
- Regular aerobic exercise: Moderate‑intensity workouts lower IL‑6 and TNF‑α while boosting neuroprotective factors.
- Stress management: Chronic stress spikes cortisol, which can paradoxically increase pro‑inflammatory cytokines. Techniques like mindfulness or yoga show modest reductions in relapse frequency.
These tweaks won’t replace disease‑modifying drugs, but they give patients a sense of control and may improve long‑term outcomes.

Targeting inflammation with next‑generation therapies
New drugs aim straight at the cytokine culprits or the cells that release them. For example, anti‑IL‑17 antibodies (like secukinumab) and B‑cell depleters (such as ocrelizumab) have shown strong reductions in relapse rates. Researchers are also testing small‑molecule inhibitors that block GM‑CSF signaling, hoping to halt the chronic feedback loop that fuels progressive disease.
Even beyond pharmaceuticals, experimental approaches like stem‑cell transplantation seek to reset the immune system, essentially giving the body a fresh start without the inflammatory baggage.
Quick takeaways
- Inflammation is the engine behind myelin loss and nerve damage in MS.
- T cells, B cells, and microglia release cytokines that breach the blood‑brain barrier.
- Key cytokines-IL‑6, TNF‑α, IFN‑γ, IL‑17, GM‑CSF-create self‑sustaining loops.
- When the barrier cracks, immune cells flood the CNS, killing oligodendrocytes and sparking demyelination.
- Chronic, low‑grade inflammation drives progressive neurodegeneration, even after relapses subside.
- Lifestyle choices-vitamin D, omega‑3s, exercise, stress control-can modestly lower inflammatory markers.
- Modern therapies target specific cytokines or B‑cells, offering clearer pathways to disease control.
Frequently Asked Questions
Can diet really affect inflammation in MS?
Yes. Studies show that higher vitamin D levels and regular intake of omega‑3 fatty acids are linked to lower relapse rates. A balanced diet low in processed sugars also helps keep cytokine spikes in check.
Why do some MS patients experience sudden relapses while others steadily decline?
The pattern depends on whether acute, high‑intensity inflammation dominates (causing relapses) or whether a low‑grade, chronic inflammation persists (driving progressive decline). Different immune pathways are more active in each scenario.
Are anti‑IL‑17 drugs safe for long‑term use?
Clinical trials report good efficacy in reducing relapses, but patients should be monitored for infections and possible skin issues. Your neurologist will weigh benefits against risks based on your disease stage.
How does the blood‑brain barrier become leaky?
Inflammatory cytokines such as IL‑6 and TNF‑α disrupt tight‑junction proteins that seal the barrier. Once these proteins weaken, immune cells slip through and set up lesions.
Can exercise worsen MS symptoms?
Moderate, regular aerobic activity tends to lower inflammatory markers and improve fatigue. Over‑exertion, however, can temporarily increase heat sensitivity, so pacing is key.





Reviews
Everything they label as “inflammation” in multiple sclerosis is just a smokescreen for a hidden agenda designed to push experimental pharmaceuticals.
It’s fascinating how the immune system can mistake myelin for a foreign invader, isn’t it? The sarcasm is not lost on me when researchers claim we can simply “tune” these cells with a pill. Yet, the underlying mechanisms involve T‑cell activation, B‑cell antibody production, and microglial response, all of which are well documented. In plain terms, the body’s own defense goes rogue, and we are left coping with the fallout.
The pathological cascade in MS epitomizes a maladaptive immunological onslaught, where Th1/Th17 polarization drives a cytokine storm that breaches the neurovascular unit. From a geopolitical standpoint, the United States must prioritize funding for high‑throughput cytokine profiling to outpace rival research programs. The intricacies of GM‑CSF signaling and its autocrine amplification loops demand a translational pipeline that only a powerhouse nation can sustain. Moreover, the dysregulation of blood‑brain barrier integrity, mediated by IL‑6‑induced tight‑junction remodeling, underscores the necessity for aggressive therapeutic intervention. In short, without a decisive national strategy, we risk ceding scientific leadership to adversarial entities.
Interesting take-still, the data suggest that vitamin D modulation correlates with reduced relapse frequency; likewise, omega‑3 intake appears to blunt cytokine surges; finally, regular aerobic activity may lower IL‑6 levels.
Oh great, another miracle cure hidden in a fish oil capsule 🐟💊-because clearly, the solution to a complex autoimmune disease is just more EPA. 🙄
The immune dysregulation observed in multiple sclerosis cannot be adequately captured by a simplistic “bad cells” narrative.
When one examines the phenotypic shift of CD4+ T lymphocytes towards a Th1/Th17 bias, it becomes evident that cytokine orchestration is both intricate and relentless.
Interleukin‑6, tumor necrosis factor‑α, and interferon‑γ act in concert to destabilize the endothelial tight junctions that compose the blood‑brain barrier.
This destabilization permits peripheral immune effectors to infiltrate the central nervous system, where they encounter oligodendrocyte progenitors.
The ensuing cytotoxic assault results in demyelination, a process that compromises saltatory conduction and manifests clinically as sensory and motor deficits.
Subsequent axonal transection initiates a cascade of neurodegenerative events that persist even after inflammatory activity subsides.
Recent longitudinal imaging studies have demonstrated that chronic, low‑grade inflammation correlates with progressive brain atrophy independent of relapse frequency.
Moreover, genome‑wide association studies reveal polymorphisms in the HLA‑DRB1 locus that predispose individuals to an exaggerated immune response.
These genetic insights underscore the necessity for personalized therapeutic strategies that target specific molecular pathways.
Anti‑IL‑17 monoclonal antibodies, for example, have shown efficacy in reducing new lesion formation, yet they carry a non‑trivial risk of opportunistic infections.
Similarly, B‑cell depleting agents such as ocrelizumab have reshaped the treatment landscape but require vigilant monitoring for hypogammaglobulinemia.
On the non‑pharmacologic front, sustained aerobic exercise has been shown to attenuate circulating IL‑6 concentrations, thereby offering an adjunctive anti‑inflammatory benefit.
Nutritional modulation, particularly adequate vitamin D status, further supports immune homeostasis by promoting regulatory T‑cell expansion.
Nevertheless, adherence to lifestyle interventions remains suboptimal in many patient cohorts, reflecting broader socioeconomic disparities.
In light of these complexities, a multi‑modal approach that integrates disease‑modifying therapies, rehabilitative services, and psychosocial support appears most prudent.
Ultimately, only through coordinated research funding, interdisciplinary collaboration, and patient‑centered care can we hope to mitigate the relentless inflammatory drive that fuels MS progression.
When you look at the cytokine network in MS, think of it like a badly tuned orchestra where the brass section (IL‑6, TNF‑α) keeps blasting while the strings (neuroprotective factors) try to stay in harmony.
First off, you want to get a baseline inflammatory panel; that tells you which players are out of line.
Second, disease‑modifying therapies such as B‑cell depleters can effectively mute the overactive brass, but they need to be paired with regular monitoring to catch any infections early.
Third, lifestyle tweaks-like getting at least 150 minutes of moderate cardio a week-lower IL‑6 levels naturally, acting like a quieting background track.
Don’t forget vitamin D; a serum level above 30 ng/mL is associated with fewer relapses, so a daily supplement can be a low‑cost side‑kick to the main treatment.
Bottom line: combine pharma, fitness, and nutrition, and you give yourself the best shot at keeping the inflammation in check.
Remember, every small step-whether it’s a brisk walk or a splash of sunshine-adds a brushstroke to the larger canvas of recovery.
Stay consistent, keep the focus on what fuels you, and let the body do its resilient work.
Your journey may feel like a marathon, but pacing yourself and celebrating tiny victories will keep the momentum alive.
Keep pushing forward, one purposeful breath at a time.