Bioequivalence Requirements: What Makes Generic Drugs Truly Equal
When you pick up a generic pill, you’re trusting that it does the same job as the brand-name version. That trust isn’t guesswork—it’s built on bioequivalence requirements, a set of scientific standards that prove a generic drug delivers the same amount of active ingredient at the same rate as the original. Also known as pharmacokinetic equivalence, these rules are enforced by the FDA to make sure you’re not getting a weaker or slower version just because it costs less. Without bioequivalence, generics could be useless—or worse, dangerous. That’s why every generic drug must pass strict tests showing it behaves the same way in your body as the brand-name drug.
These tests don’t just check the pill’s ingredients. They measure how fast and how much of the drug enters your bloodstream—called drug absorption, the process by which a medication moves from the digestive tract into the blood. If a generic drug absorbs too slowly, it won’t work fast enough. If it absorbs too quickly, it might cause side effects. The acceptable range? Usually within 80% to 125% of the brand-name drug’s levels. That’s not a guess—it’s a tightly controlled window backed by clinical data from hundreds of volunteers.
Not all generics are created equal, though. authorized generics, the exact same drug made by the brand company but sold under a generic label are identical in every way, down to the inactive ingredients. Traditional generics, while still FDA-approved, can have different fillers or coatings that affect how they break down in your stomach. That’s why some people swear their generic doesn’t work as well—it’s not always in their head. It’s sometimes in the formulation. And that’s why understanding FDA approval, the legal and scientific process that ensures generics meet safety and performance standards matters more than ever.
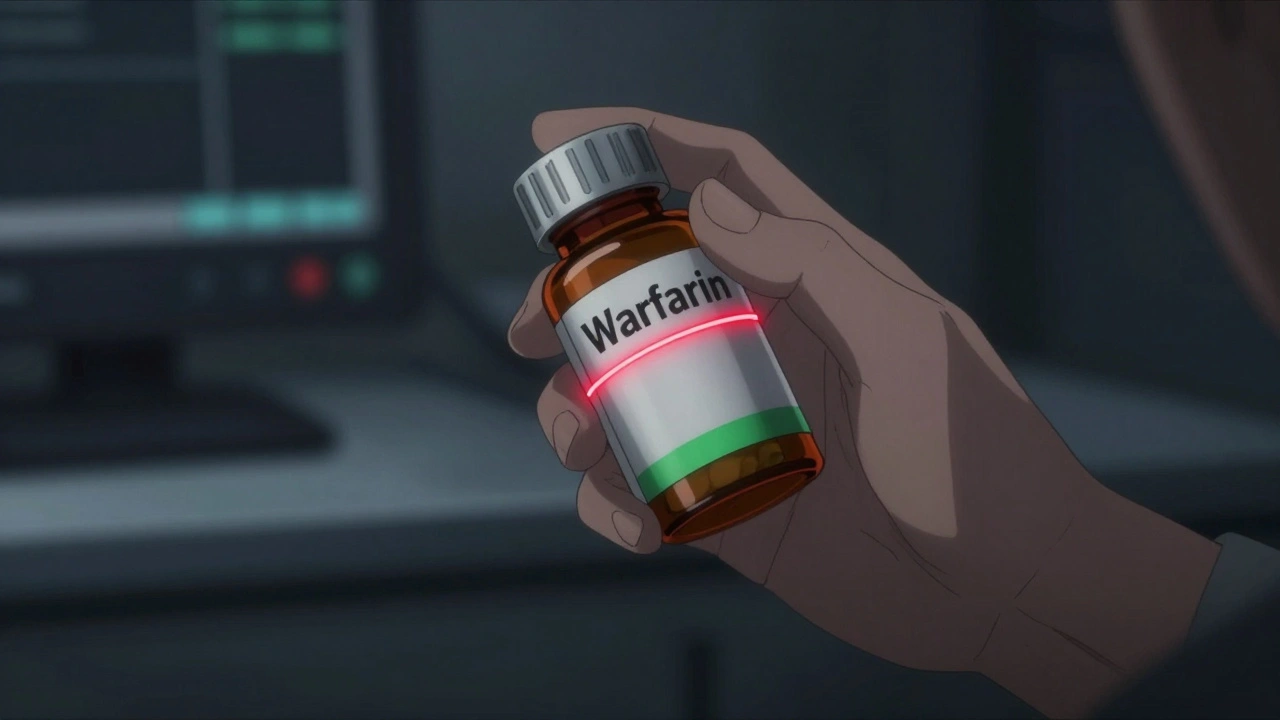
These rules apply to most pills, but not all. Drugs with a narrow therapeutic index—like warfarin or lithium—need even tighter controls because tiny differences can cause serious harm. That’s why you’ll see more scrutiny on those. Meanwhile, for common meds like lisinopril or metformin, bioequivalence is well-established and reliable. The system works—but only if you know what to look for.
What you’ll find in the posts below isn’t just theory. It’s real stories from people who’ve switched generics, got confused by labels, or wondered why one pill felt different than another. You’ll learn how to tell if your generic is truly equivalent, why some pharmacies switch brands without warning, and how to ask your pharmacist the right questions. This isn’t about saving a few dollars—it’s about making sure your treatment still works.