Betamethasone Dosage Calculator
Calculate Betamethasone Dosage
Recommended Dosage Range
Additional Information
Warning: This dosage is outside the typical recommended range. Consult with a veterinarian before administration.
When a pet or a farm animal develops swelling, itching, or an autoimmune flare‑up, veterinarians often turn to a class of drugs called corticosteroids. Among them, betamethasone veterinary has become a go‑to for fast, potent anti‑inflammatory action. This guide walks you through what betamethasone is, how it works in different species, the typical dosage forms you’ll see in a clinic, safety considerations, and how it stacks up against other common veterinary steroids.
What Is Betamethasone?
Betamethasone is a synthetic glucocorticoid that mimics the body’s natural cortisol hormone. It was first synthesized in the 1950s and quickly adopted for human dermatology because of its high anti‑inflammatory potency and minimal mineralocorticoid activity. In veterinary medicine, the same properties translate into rapid control of swelling, itching, and immune‑mediated conditions across a wide array of species.
Because betamethasone binds strongly to glucocorticoid receptors, it suppresses the release of inflammatory mediators like prostaglandins and cytokines. The drug’s half‑life in animals varies by route-intramuscular injections can linger for 24‑48 hours, while topical creams act locally for a few hours before being absorbed.
How Betamethasone Works in Animals
Glucocorticoid receptors are present in virtually every cell type, from skin fibroblasts to immune white blood cells. When betamethasone engages these receptors, it triggers a cascade that:
- Reduces the transcription of genes encoding inflammatory proteins.
- Promotes the production of anti‑inflammatory proteins such as annexin‑1.
- Inhibits the migration of immune cells to sites of injury.
One key advantage for veterinarians is the drug’s ability to be administered systemically (injection or oral) for whole‑body conditions, or topically for localized skin lesions. The flexibility allows clinicians to tailor treatment to the animal’s size, species, and the severity of the problem.
Common Veterinary Indications
Betamethasone shows up in treatment protocols for a surprisingly broad list of conditions. Here are the most frequent uses across companion and farm animals:
- Dermatologic disorders: pyoderma, allergic dermatitis, and hot spots in dogs and cats.
- Musculoskeletal inflammation: osteoarthritis flare‑ups in horses, dogs, and goats.
- Immune‑mediated diseases: pemphigus foliaceus in felines, autoimmune hemolytic anemia in dogs, and immune‑mediated polyarthritis in cattle.
- Respiratory issues: asthma‑like airway inflammation in cats and chronic bronchitis in horses.
- Ophthalmic conditions: uveitis and severe conjunctivitis in equine and canine patients (usually as an ophthalmic suspension).
Because the drug is powerful, veterinarians reserve it for cases where non‑steroidal anti‑inflammatories (NSAIDs) have failed or where rapid symptom control is essential.
Dosage Forms and Administration
Betamethasone is available in several formulations that affect how quickly it acts and how long the effect lasts. The choice depends on the species, the condition, and the owner’s ability to comply with a dosing schedule.
- Injectable solution (0.5 mg/mL or 4 mg/mL): Often used for acute flare‑ups in dogs, cats, and horses. Administered intramuscularly (IM) or intravenously (IV) for rapid systemic effect. Typical dosage ranges from 0.05-0.1 mg/kg IM every 24-48 hours.
- Topical cream or ointment (0.05 %-0.1 %): Ideal for localized skin lesions in small animals. Apply a thin layer to the affected area 1-2 times daily, avoiding contact with mucous membranes.
- Ophthalmic suspension (0.1 %): Used for uveitis in horses and dogs. Instill one to two drops in the affected eye every 12 hours.
- Oral tablets (1 mg or 5 mg): Less common due to variable absorption, but useful for chronic conditions in larger animals where injections are impractical.
Veterinarians must adjust the dose for pregnant animals, geriatric patients, and those with compromised liver or kidney function. Always follow the prescribing label and consider therapeutic drug monitoring when high cumulative doses are required.
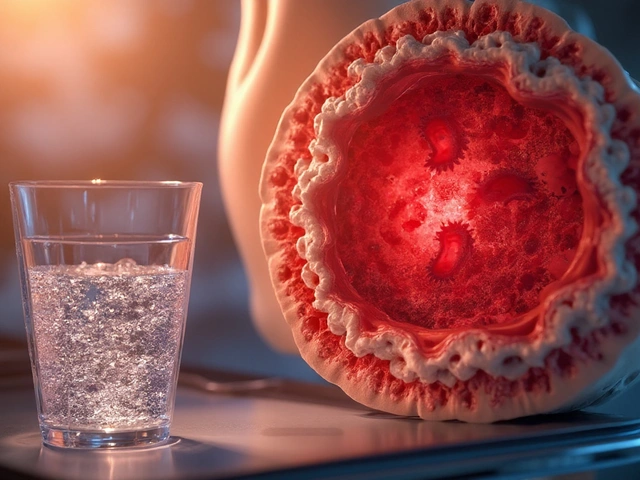
Safety, Side Effects, and Contra‑Indications
Like any potent steroid, betamethasone carries a risk profile that demands careful management. The most frequently reported adverse effects in animals include:
- Gastrointestinal ulceration: Especially in dogs and horses receiving high‑dose IM injections.
- Pancreatitis: Reported in some predisposed dog breeds after systemic exposure.
- Immune suppression: Increases susceptibility to secondary bacterial or fungal infections.
- Endocrine disruption: Long‑term use can suppress the hypothalamic‑pituitary‑adrenal (HPA) axis, leading to adrenal insufficiency upon abrupt withdrawal.
- Delayed wound healing: Topical application over open wounds can impede tissue regeneration.
Contra‑indications are relatively clear: do not use betamethasone in animals with active, uncontrolled infections, known hypersensitivity to corticosteroids, or severe systemic fungal disease. In pregnant bitches, the drug can affect fetal development, so it should be avoided unless the benefit markedly outweighs the risk.
To mitigate risks, veterinarians often employ a tapering schedule when discontinuing therapy, prescribe gastro‑protectants (e.g., famotidine) alongside high‑dose regimens, and recommend regular blood work to monitor glucose, liver enzymes, and complete blood counts.
Comparison with Other Veterinary Corticosteroids
Betamethasone isn’t the only steroid in the vet’s toolbox. Below is a quick side‑by‑side look at how it stacks up against two other popular options: dexamethasone and prednisolone.
| Attribute | Betamethasone | Dexamethasone | Prednisolone |
|---|---|---|---|
| Potency (relative to cortisol) | 25‑30 × | 30‑35 × | 4‑5 × |
| Mineralocorticoid activity | Very low | Very low | Moderate |
| Typical IM dose (mg/kg) | 0.05‑0.1 | 0.02‑0.05 | 0.5‑1.0 |
| Half‑life (hours) | 12‑24 | 36‑72 | 2‑4 |
| Common species use | Dogs, cats, horses, cattle | Horses, livestock (anti‑inflammatory) | Small animals, birds |
| Cost (US $ per 5 mg dose) | ~2.50 | ~3.00 | ~1.20 |
Betamethasone offers a middle ground: it’s more potent than prednisolone but less costly than dexamethasone, and its relatively low mineralocorticoid activity makes it safer for animals prone to fluid retention. However, for ultra‑long‑acting needs-such as chronic joint disease in horses-dexamethasone’s extended half‑life might be preferable.
Practical Tips & Best Practices
Here are some field‑tested pointers that help you get the most out of betamethasone while keeping your patients safe:
- Start low, go slow: Begin with the minimum effective dose and only increase if clinical signs persist after 24‑48 hours.
- Rotate injection sites: For horses, alternate between the gluteal muscles and the neck to reduce local tissue irritation.
- Combine with a proton pump inhibitor if the animal has a history of gastric ulcers-famotidine at 0.5 mg/kg PO q12h works well.
- Monitor blood glucose in diabetic dogs; corticosteroids can trigger hyperglycemia.
- Document the taper plan in the animal’s medical record. A typical taper might reduce the dose by 20 % every 3‑5 days.
- Avoid abrupt cessation after more than 7‑10 days of therapy; withdrawal can cause adrenal crisis.
- Educate owners about signs of infection (fever, lethargy) and when to call the clinic.
By integrating these habits into routine practice, you’ll see quicker recovery times and fewer complications, which keeps both the animal and the owner happy.
Frequently Asked Questions
Can betamethasone be used in pregnant animals?
Generally, no. Betamethasone can cross the placenta and may affect fetal development. It should only be used if the therapeutic benefit far outweighs the potential risk, and then at the lowest effective dose.
How long does the anti‑inflammatory effect last after an IM injection?
The clinical effect usually persists for 24‑48 hours, though the drug’s half‑life can stretch up to 24 hours in most species. Some horses may experience relief for up to 72 hours.
Is it safe to give betamethasone together with antibiotics?
Yes, combining a corticosteroid with an appropriate antibiotic is common practice when an infection is suspected, as the steroid can mask signs of infection. Choose an antibiotic that covers secondary bacterial pathogens and monitor the animal closely.
What are the signs of adrenal insufficiency after stopping betamethasone?
Signs include lethargy, vomiting, weakness, and low blood pressure. If you see these symptoms within a week of abrupt discontinuation, start a low‑dose glucocorticoid and consult your veterinarian.
Can betamethasone be used topically on open wounds?
It’s not recommended. Steroids can delay granulation tissue formation and increase infection risk. Reserve topical use for intact skin or superficial lesions only.
These answers cover the most common concerns you’ll hear from pet owners and farm managers. Keep them handy for quick reference during consultations.
Betamethasone remains a versatile, powerful tool in the veterinary arsenal. By respecting its potency, dosing it correctly, and staying vigilant for side effects, you can provide rapid relief for a wide range of animal patients while minimizing risk.




Reviews
Betamethasone is just another pharma trick to keep vets under Big Pharmas thumb.
The guide tries to sound scientific, but it glosses over the long‑term bone loss that steroids can cause. Owners often think a quick shot is harmless, yet the reality is far from that. You should be questioning why we rely so heavily on synthetic hormones instead of holistic care. The dosage tables are okay, but they lack warnings about adrenal collapse. It’s definately a missed opportunity to educate practitioners on safer alternatives.
While the cautions are valid, we also have to weigh the animal’s immediate suffering against the theoretical risks. In many acute flare‑ups, withholding a potent anti‑inflammatory could mean prolonged pain. The guide’s emphasis on monitoring is a pragmatic compromise. It invites clinicians to reflect on the ethics of pain relief versus potential side effects. Ultimately, the decision rests on a case‑by‑case assessment.
The misuse of betamethasone reflects a deeper moral decay in veterinary practice. When profit drives prescription, animals become mere lab rats for pharmaceutical giants. This guide attempts to sanitize that narrative with glossy tables and cost comparisons, but it sidesteps the ethical breach of silencing adverse outcomes. Veterinarians must reclaim their oath to do no harm, not bow to corporate incentives. Our duty is to champion transparent, compassionate care, lest we betray the very beings we swear to protect.
Great summary! 👍 It’s clear and easy to follow, especially for new vets. The tables help a lot. 😊 Keep it up!
Love this guide 🙌 it covers everything from dosages to safety tips 😊 the tables are super helpful 🤓 looking forward to more posts like this 🚀
While the enthusiasm is appreciated, it’s crucial to remember that each animal reacts uniquely. Over‑enthusiasm can lead to over‑medication, which may mask underlying issues. Let’s keep the discussion grounded in evidence and patient welfare.
Reading through the guide reminds me of the delicate balance between intervention and natural healing. On one hand, the pharmacology is undeniably powerful; on the other, we risk tipping the scales toward dependency. It’s a reminder that our role is not just to treat symptoms but to steward the overall health trajectory of the animal. Each dosage decision carries weight beyond the immediate flare‑up, influencing endocrine stability and immune resilience. As clinicians, we must cultivate both scientific rigor and compassionate wisdom.
The guide is thorough, yet a concise summary of tapering protocols would aid quick reference.
Betamethasone remains a cornerstone in managing acute inflammatory crises across species, thanks to its high glucocorticoid potency and minimal mineralocorticoid activity.
Its rapid onset, typically within hours after intramuscular injection, can dramatically reduce edema and pruritus, providing much‑needed relief for distressed patients.
However, the very qualities that make it effective also underpin its risk profile, necessitating vigilant monitoring of gastrointestinal, metabolic, and endocrine parameters.
For canine patients, a common starting dose of 0.05 mg/kg IM every 24 hours strikes a balance between efficacy and safety, yet clinicians must adjust for breed‑specific sensitivities such as a predisposition to pancreatitis in miniature schnauzers.
Equine practitioners often favor the 4 mg/mL injectable formulation for joint flare‑ups, but they should rotate injection sites and pair the steroid with a gastro‑protectant to mitigate ulcer formation.
In dairy cattle, the drug’s immunosuppressive effects can reduce mastitis severity, but withdrawal times must be strictly observed to prevent residue violations in milk.
Topical preparations, ranging from 0.05 % to 0.1 % concentrations, are ideal for localized dermatologic lesions, yet they should never be applied to open wounds where healing is already compromised.
Ophthalmic suspensions demand meticulous administration, as improper dosing can precipitate intra‑ocular pressure spikes, especially in predisposed breeds.
The half‑life of betamethasone, averaging 12–24 hours, informs the tapering schedule; a typical protocol reduces the dose by 20 % every three to five days to allow the hypothalamic‑pituitary‑adrenal axis to recover.
Blood work should be performed before initiating therapy and periodically thereafter, focusing on glucose, liver enzymes, and complete blood counts to catch early signs of adverse effects.
For diabetic dogs, concurrent insulin adjustments may be required because corticosteroids can provoke hyperglycemia.
When used in pregnant bitches, the drug crosses the placenta, so the risk–benefit ratio must be carefully weighed and, if possible, alternative therapies should be explored.
Cost considerations also play a role; while betamethasone is generally less expensive than dexamethasone, the total expense of adjunctive medications and monitoring can add up.
Ultimately, the decision to employ betamethasone should hinge on a comprehensive assessment of the animal’s condition, the owner’s capacity for follow‑up, and the practitioner’s familiarity with the drug’s nuances.
By adhering to these best‑practice guidelines, veterinarians can harness the drug’s therapeutic power while safeguarding against its potential pitfalls.
Thank you for the thorough overview. The step‑by‑step tapering guidance is especially useful. I’ll incorporate these checkpoints into my practice.
The exposition is solid, yet I must stress that any deviation from the recommended monitoring can lead to severe complications. Veterinarians must enforce strict adherence to the protocol without compromise.