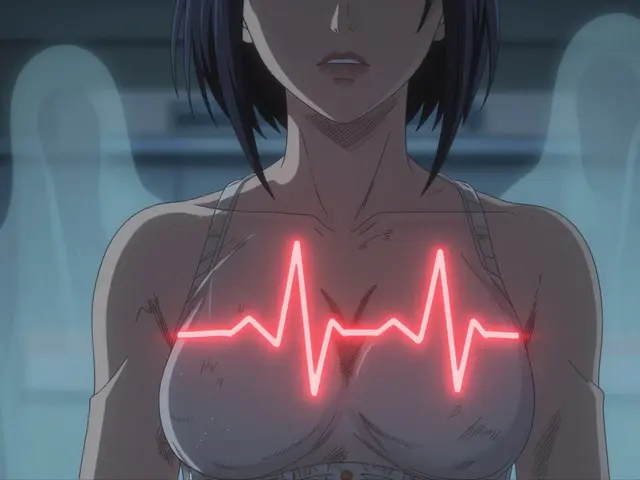
When a drug safety alert pops up-whether it’s a recall notice, a warning about side effects, or an emergency update from the FDA-you don’t have time to freeze. Your heart races. Your breath gets shallow. Your mind spins through worst-case scenarios. That’s not weakness. That’s biology. Your brain’s alarm system is firing, and if you don’t interrupt it, you’ll make decisions based on fear, not facts.
Why Panic Makes Alerts Worse
Panic doesn’t help you act faster. It makes you slower. When you’re flooded with stress, your amygdala-the part of your brain that sounds alarms-takes over. Meanwhile, your prefrontal cortex, the part that weighs options and thinks ahead, shuts down. Studies show this cuts your ability to think clearly by up to 67%. You might skip checking the source, ignore details, or rush into actions that make things worse. In drug safety, that’s dangerous. You might stop a life-saving medication because of a vague alert. Or you might ignore a real risk because you’re too overwhelmed to read the fine print. Either way, panic turns a manageable situation into a crisis.Stop the Panic in 90 Seconds
The goal isn’t to eliminate stress. It’s to bring your thinking brain back online-fast. Here’s how:- Use the 4-7-8 breathing technique: Breathe in for 4 seconds, hold for 7, exhale slowly for 8. Repeat three times. This lowers your heart rate from 110+ bpm to 70-85 bpm within 90 seconds, calming your nervous system. It’s not magic-it’s physiology.
- Apply cold to your face: Splash your face with cold water (10-15°C) or hold an ice pack to your cheeks for 20 seconds. This triggers the mammalian dive reflex, which instantly slows your heart and resets your stress response.
- Do 30 seconds of intense movement: Jump in place, march hard, or shake out your arms. This burns off adrenaline and breaks the cycle of freeze-or-flee.
Ground Yourself Before You Act
After you’ve calmed your body, you need to ground your mind. Anxiety pulls you into the future-imagining disasters that haven’t happened. Grounding brings you back to now. Use the 5-4-3-2-1 method:- Find 5 things you can see (the clock, your coffee mug, the window, the text on your screen, the pen on your desk).
- Touch 4 things (your chair, your phone, your shirt fabric, your keys).
- Listen for 3 sounds (the hum of the computer, distant traffic, your own breath).
- Smell 2 things (your toothpaste, the air, your hand lotion).
- Taste 1 thing (sip water, chew gum, take a mint).

Ask the Right Questions
Now that you’re calm and present, it’s time to act. But not just any action. The right action. Use this simple filter before you do anything:- What’s the source? Is this from the FDA, EMA, or a legitimate health agency? Or is it a blog post, social media rumor, or spam email? Check the official website. Don’t trust screenshots.
- What’s the risk level? Alerts are graded. Look for words like “urgent,” “serious,” or “warning.” A “precaution” is not the same as a “recall.”
- Who does this affect? Is it for all users? Only those over 65? Only people taking it with another drug? Don’t assume it applies to you.
- What’s the alternative? If you’re considering stopping a medication, what happens if you do? What happens if you don’t? Talk to your pharmacist or doctor-but don’t wait days. Many pharmacies offer same-day consultations.
- Does this align with my health goals? Are you managing high blood pressure? Diabetes? Chronic pain? Does stopping this drug help or hurt that goal? Write it down if you need to.
Prepare Before the Alert Hits
Waiting until the alarm sounds to learn how to respond is like practicing a fire drill during a real fire. You need to train ahead of time.- Practice daily: Spend 10 minutes a day doing breathing or grounding exercises. Not because you’re anxious-but because you want to stay calm when something happens. Research shows just eight weeks of daily mindfulness increases gray matter in your decision-making brain region by 4.3%.
- Build a quick-reference kit: Keep a small folder or note on your phone with: your doctor’s number, your pharmacy’s emergency line, the FDA’s alert website, and a printed copy of the 5-4-3-2-1 method. Add a mint gum or textured stone-something you can touch or taste to ground yourself.
- Limit stimulants: Caffeine, sugar, and alcohol raise baseline anxiety. If you’re on 300mg of caffeine daily, you’re already primed for panic. Cut it to 200mg or less. Sleep 7-9 hours. Move 150 minutes a week. These aren’t “nice-to-haves.” They’re your first line of defense.
- Journal your alerts: After every alert-even if it turns out to be nothing-write down: What triggered it? How did you feel? What did you do? What worked? Over time, you’ll spot patterns and build your own playbook.

It’s Not Just You
You’re not alone in this. In 2023, the average person received 67 digital alerts per week-from banks, phones, health apps, weather, security, and now drug safety systems. That’s over 3,500 alerts a year. Your brain wasn’t built for that. That’s why health systems are changing. The European Union’s DORA law, effective January 2025, now requires drug safety systems to include “human factor considerations.” Hospitals, pharmacies, and insurers are training staff in panic response. AI-powered alert systems are being built to detect when a user’s heart rate spikes and automatically pause the alert to guide them through breathing exercises first. This isn’t futuristic. It’s necessary. And you don’t have to wait for systems to catch up. You can start today.What to Do When You Get an Alert
Here’s your simple, step-by-step routine:- Pause. Don’t click. Don’t react. Just stop.
- Breathe. Do 4-7-8 breathing for one cycle.
- Ground. Use 5-4-3-2-1.
- Verify. Go to the official source (FDA.gov, EMA.europa.eu, your national health agency).
- Ask. Use the five questions above.
- Act. Only after you’ve answered them.
What if I’m still too anxious to follow the steps?
If you’re too overwhelmed, start with just one thing: cold water on your face or 30 seconds of jumping jacks. Even one small physical action breaks the panic cycle. Once your body calms down, your mind follows. Don’t try to do everything at once. Do one step. Then the next. Progress, not perfection.
Should I stop my medication right away if there’s an alert?
Never stop a prescribed medication without talking to your doctor or pharmacist. Many alerts are precautionary or apply only to specific groups. Stopping suddenly can be more dangerous than the alert itself. For example, abruptly stopping blood pressure or antidepressant meds can cause rebound effects. Always verify the alert’s scope and consult a professional before changing your regimen.
How do I know if an alert is real or fake?
Legitimate alerts come from official sources: FDA, EMA, Health Canada, TGA (Australia), or your national health authority. Never trust alerts sent via unsolicited email, text, or social media DMs. Go directly to the agency’s website. Look for official logos, secure URLs (https://), and publication dates. If it’s urgent, the agency will post it on their homepage and issue a press release.
Can I rely on my pharmacist for help during an alert?
Yes. Pharmacists are trained to interpret drug safety alerts and advise patients on next steps. Many offer same-day phone or in-person consultations. Keep your pharmacy’s contact info saved in your phone. If you’re unsure about an alert, call them before doing anything else. They’re often the fastest, most reliable source of accurate guidance.
Is this advice only for people with anxiety disorders?
No. These techniques work for everyone. Panic is a universal human response to sudden threats-not a personality flaw. Even people who consider themselves calm can freeze under pressure. These tools are like seatbelts: you don’t need to be in a crash to wear one. Practicing them regularly makes you more resilient, no matter your baseline anxiety level.





Reviews
So let me get this straight-you’re telling me I should breathe and touch my coffee mug when the FDA says my blood pressure med might cause alien abduction? 😂
Meanwhile, Big Pharma’s been hiding side effects for decades and now they want me to trust their alerts? Nah. I’m not falling for the calming breathing scam. This is all a distraction tactic so they can keep selling toxic pills while we’re too busy counting our fingers to notice the real problem.
You’re not alone in feeling overwhelmed-and that’s okay. What you’re experiencing is completely normal. The techniques in this post aren’t just ‘tips’-they’re science-backed lifelines. I’ve used the 5-4-3-2-1 method during my own panic attacks after a medication alert, and it literally saved me from calling my doctor in a frenzy. You don’t need to be perfect. Just start with one breath. One step. You’ve got this. 💪
Too long
Didn’t read
Just stop taking meds if you’re scared
Oh my goodness, this is so important-and so beautifully laid out! 🌟
Thank you for writing this with such clarity, compassion, and precision! I’ve been a pharmacist for 18 years, and I can’t tell you how many patients I’ve seen panic and stop life-saving meds because of a vague Facebook post. The 4-7-8 breathing technique? Yes! The grounding method? Absolutely! And the reminder to verify the source? CRITICAL.
Every single person reading this needs to print this out and tape it to their fridge. Or save it as a note on their phone. Or text it to their mom. Please. This is public health gold.
Also-please don’t ignore the caffeine warning. I’ve had patients on 8 espressos a day wonder why they’re ‘always anxious.’ Honey, your nervous system is a shaken soda can.
Thank you. Thank you. Thank you.
Kinda makes sense
But I still don’t trust the FDA
When I got my first drug alert last year, I was a mess-heart pounding, hands shaking, ready to toss my entire medicine cabinet out the window.
Then I remembered the cold water trick. I splashed my face, felt the shock of it, and just… stopped.
Not because I was calm. But because my body finally stopped screaming.
That’s when I called my pharmacist. She told me the alert only applied to people on high doses with kidney issues-and I wasn’t one of them.
I cried. Not from fear. From relief.
You don’t need to be a superhero to handle this. You just need to pause. One breath. One step. One human moment.
And you’re already doing better than you think.
Ah yes, the classic Western wellness-industrial complex solution: breathe, touch things, and trust the state-sanctioned pharmaceutical narrative.
Meanwhile, in India, we’ve been using Ayurvedic grounding techniques for millennia-like pranayama and walking barefoot on earth-which actually address root causes rather than symptoms.
Also, the FDA is a corporate puppet. Why do you think they only issued alerts after 200+ deaths? Classic delayed reaction to protect profits.
These ‘techniques’ are just placebo bandaids on a bullet wound.
Also, I meditate in a cave. You should too. 🙏
I appreciate the intent behind this post. It’s thoughtful. And the science is sound.
That said, I think we need to be careful about framing panic as something to be ‘fixed’ with techniques. For some of us, panic is a signal-not a malfunction.
Maybe the system is broken. Maybe the alerts are too frequent. Maybe the information is too opaque.
It’s not just us being weak. It’s the environment being overwhelming.
So yes, breathe. But also: demand better systems.
Because no amount of grounding will fix a broken alert infrastructure.
good post but u misspelled 'precaution' in the first paragraph
also the 4-7-8 thing works but i use 5-6-7 its better
and dont forget to drink water after
also i heard from my cousin who works at a hospital that some alerts are fake to sell more meds
so always check 3 sources not just one
and dont trust the FDA they got money from pharma
but still this post is good for newbies
This is one of the most balanced, practical, and human-centered pieces on health alerts I’ve read in years.
It doesn’t dismiss fear. It doesn’t glorify stoicism. It meets people where they are-with science, empathy, and actionable steps.
The fact that you included the pharmacist’s role and the importance of sleep and caffeine? That’s the kind of detail most medical content ignores.
Thank you for writing this. I’m sharing it with my entire family.
And yes-I’m printing the 5-4-3-2-1 list and taping it to my bathroom mirror.
So let me summarize: when the world tries to scare you, just… breathe? And touch your keys?
Wow. What a revolutionary concept.
Meanwhile, the pharmaceutical industry is lobbying to make drug alerts mandatory on every smart device, while simultaneously suppressing independent research on side effects.
So yes, by all means-take a deep breath while the system quietly rewrites your rights.
Maybe next time, they’ll tell us to hug a tree before we get a cancer warning.
Oh wait-they already did.
Thanks for the laugh. I needed that.
When I read this, I felt like someone finally understood how heavy this all is.
Not just the meds. Not just the alerts.
But the loneliness of being the one who has to remember everything.
The one who Googles at 2 a.m.
The one who wonders if they’re overreacting-again.
This didn’t just give me steps.
It gave me permission to be human.
Thank you.
I’m crying. Not because I’m scared.
Because I’m not alone anymore.
As someone who works in global health communications, I can say with absolute certainty: this post is a model for how to communicate high-stakes medical information with both rigor and humanity.
The 5-4-3-2-1 grounding technique? Used by trauma teams in war zones. The 4-7-8 breath? Taught in NASA flight training for pilot stress management.
And the emphasis on verifying sources? Crucial in an age of AI-generated fake alerts.
But what I love most is how you normalize the panic-not as a flaw, but as a biological response to information overload.
And the fact that you included cultural context (DORA, global agencies)? That’s rare.
This isn’t just advice.
This is public health advocacy done right.
Everyone should read this. Twice.