FDA Bioequivalence: What It Means for Generic Drugs and Your Health
When you hear FDA bioequivalence, the scientific standard that proves a generic drug performs the same as its brand-name version in the body. Also known as bioequivalent drug approval, it’s the reason your pharmacist can swap your brand-name pill for a cheaper generic without risking your health. This isn’t just paperwork—it’s a strict test that measures how fast and how much of the drug enters your bloodstream. If the generic doesn’t match the brand within tight limits, it doesn’t get approved. The FDA doesn’t guess. It runs real studies with real people, tracking blood levels over time to make sure the drug behaves the same way.
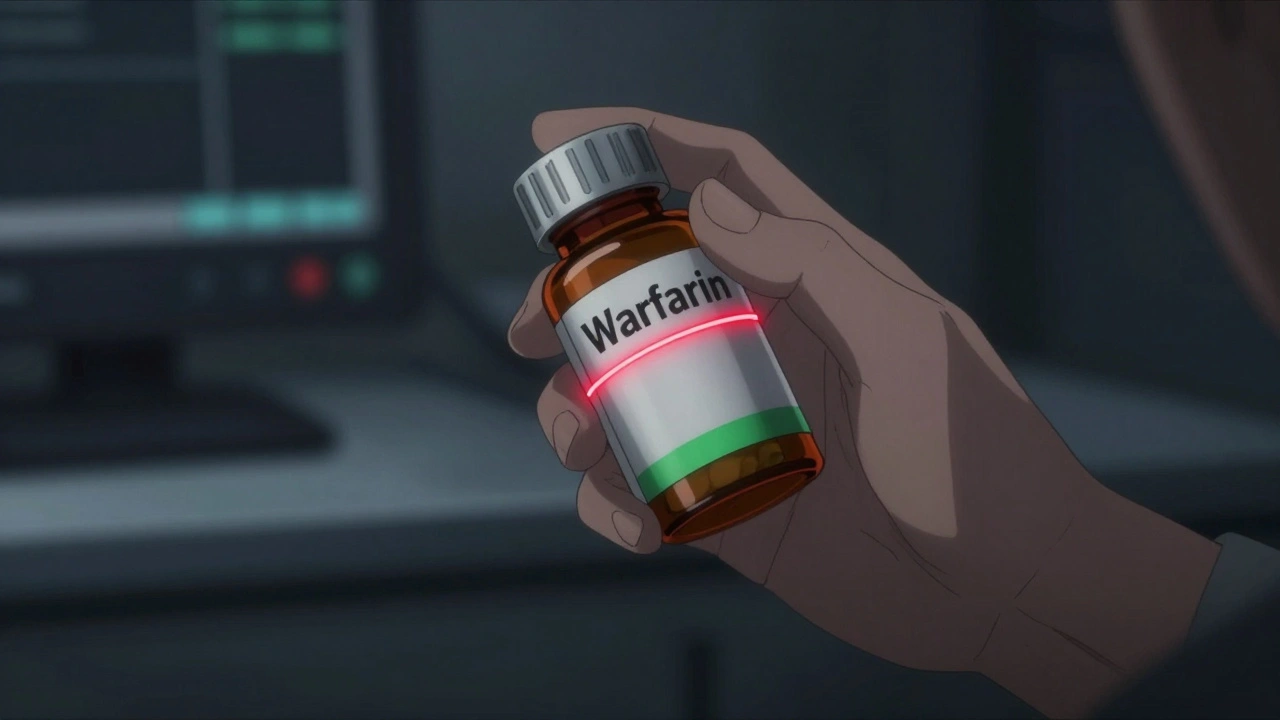
FDA bioequivalence isn’t about the pill’s color, shape, or taste. It’s about what happens inside you. The active ingredient must be identical, and the way it’s released and absorbed must be nearly the same. That’s why some generics work better for you than others—not because they’re different drugs, but because the inactive ingredients (like fillers or coatings) can affect how quickly the medicine dissolves. This is especially critical for drugs with a narrow therapeutic window, like warfarin or lithium, where even small changes in absorption can cause serious side effects. That’s also why the FDA requires extra scrutiny for these drugs, and why you might notice your doctor prefers a specific generic brand.
It’s easy to think generics are just copies. But they’re not. They’re proven to be the same in action. The ANDA approval process, the legal pathway the FDA uses to review generic drugs under the Hatch-Waxman Act. Also known as Abbreviated New Drug Application, it lets companies skip expensive animal and human trials because they’re proving equivalence, not inventing something new. This system keeps prices low without cutting corners. But perception still trips people up. If your brand-name drug made you feel better, and the generic doesn’t seem to, it’s often not the drug—it’s your brain. The nocebo effect is real. You expect less from a cheaper pill, so your body reacts as if it’s less effective. That’s why studies show people report more side effects from generics—even when they’re taking the exact same medicine under a different label.
And here’s the thing: bioequivalence doesn’t mean every generic is perfect for everyone. Some people respond better to one manufacturer’s version over another, even if both meet FDA standards. That’s why your doctor or pharmacist might stick with the same generic brand. It’s not about preference—it’s about consistency. If you’ve been stable on one, switching to another could throw off your balance, especially with blood pressure, thyroid, or seizure meds.
What you’ll find in the posts below are real stories and clear explanations about how bioequivalence affects your daily life. From why some generics feel different to how the FDA catches unsafe versions, from the truth about authorized generics to how your body reacts to the same drug in different packaging. You’ll see how this technical process connects to your health, your wallet, and your peace of mind. No jargon. No fluff. Just what you need to know to trust your meds—and know when to ask questions.