Grapefruit and Warfarin: What You Need to Know About This Dangerous Interaction
When you take warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, artificial heart valves, or deep vein thrombosis. Also known as Coumadin, it's one of the most common NTI drugs — narrow therapeutic index medications where even tiny changes in dose can lead to serious harm. Grapefruit, on the other hand, isn’t just a healthy breakfast fruit — it’s a silent disruptor of how your body processes warfarin and many other drugs.
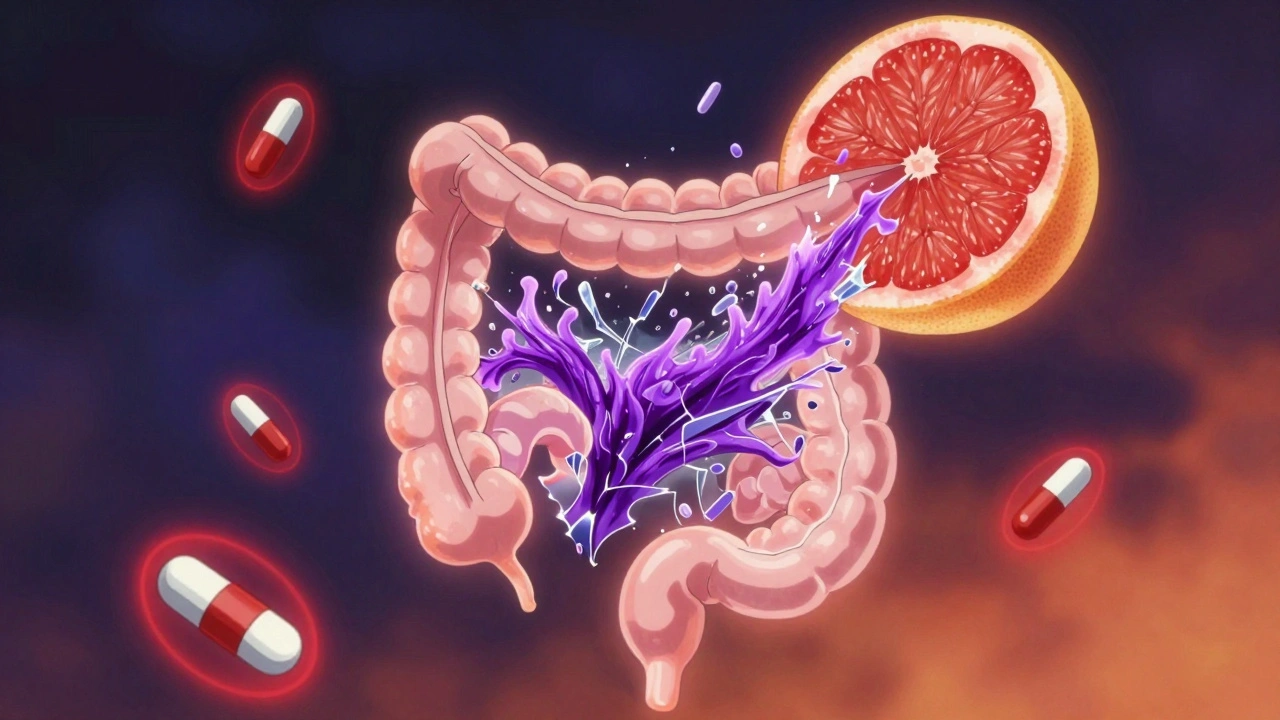
The problem isn’t that grapefruit contains warfarin. It’s that grapefruit blocks an enzyme in your gut called CYP3A4, which normally breaks down warfarin before it enters your bloodstream. When that enzyme is slowed down, more warfarin gets absorbed — making your blood thinner stronger than intended. This raises your risk of dangerous bleeding — nosebleeds, bruising, internal bleeding, even stroke. But here’s the twist: sometimes grapefruit can make warfarin less effective by altering how your liver handles it over time. Either way, your INR levels (the test that measures how long your blood takes to clot) can swing unpredictably. No one can guess how your body will react — and that’s why doctors tell you to avoid grapefruit entirely if you’re on warfarin.
This isn’t just about grapefruit juice. It’s also about whole grapefruit, pomelo, Seville oranges, and even some dietary supplements that contain grapefruit extract. It doesn’t matter if you drink it in the morning and take your pill at night — the enzyme-blocking effect lasts over 24 hours. Even if you’ve been drinking grapefruit juice for years while on warfarin, that doesn’t mean it’s safe. Your body changes. Your dose changes. The interaction doesn’t care about your routine.
People on warfarin often hear about vitamin K, antibiotics, or NSAIDs affecting their levels — but grapefruit is rarely mentioned in casual advice. Yet, it’s one of the most dangerous food-drug interactions out there. A single glass of juice can cause your INR to spike within days. And because warfarin is an NTI drug, there’s no room for error. That’s why the FDA, EMA, and Health Canada all flag grapefruit as a high-risk interaction in their guidelines for drugs like warfarin, lithium, and digoxin.
You don’t need to give up citrus forever. Oranges, tangerines, and lemons are safe. But if you love grapefruit, talk to your pharmacist or doctor. They can check your INR history and see if you’ve had unexplained spikes. Some patients switch to newer blood thinners like apixaban or rivaroxaban — which don’t interact with grapefruit — and find their lives much simpler. But if you’re staying on warfarin, the rule is simple: skip the grapefruit. No exceptions. No "just a little." Your life depends on keeping your dose stable.
Below, you’ll find real patient experiences, clinical insights, and practical tips on managing warfarin safely — from avoiding hidden grapefruit in smoothies to understanding why generic versions of warfarin require extra caution due to their narrow therapeutic window. This isn’t theoretical. It’s life-or-death stuff. And you deserve to know exactly how to protect yourself.