CYP450 Interactions: How Drugs, Food, and Genetics Affect Your Medications
When you take a pill, your body doesn’t just absorb it—it CYP450, a family of liver enzymes that break down most medications and some supplements. Also known as cytochrome P450 enzymes, these proteins act like your body’s main drug processors. If they’re slowed down or sped up, your medication can become ineffective, toxic, or cause unexpected side effects. This isn’t just about pills interacting with each other—it’s about what you eat, what you smoke, even your genes.
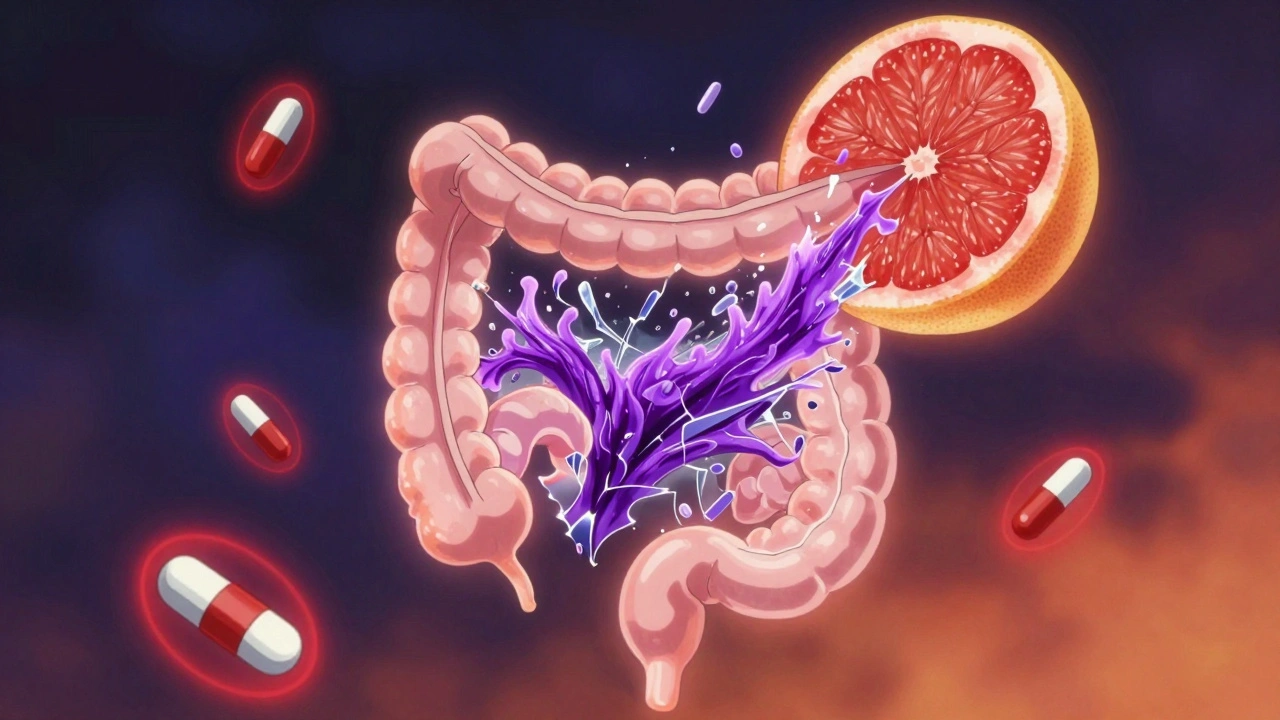
Think of CYP450 as a busy factory. Some drugs, like grapefruit juice or the antibiotic clarithromycin, jam the machinery, making it harder for your body to clear other meds. Others, like St. John’s wort or rifampin, turn the factory into overtime mode, flushing out your drugs before they can do their job. That’s why someone on warfarin might suddenly bleed after eating a big bowl of grapefruit, or why a depression pill stops working after starting an herbal supplement. These aren’t random accidents—they’re predictable drug interactions, changes in how medications behave in the body due to enzyme activity. And they’re not rare: over 70% of commonly prescribed drugs rely on CYP450 enzymes for metabolism.
Your genes play a big role too. pharmacogenomics, the study of how genes affect how your body responds to drugs explains why two people taking the same dose of a drug can have totally different outcomes. Some people are fast metabolizers—their CYP450 enzymes work overtime, so meds don’t last long. Others are slow metabolizers, and even a normal dose can build up to dangerous levels. That’s why lithium, clopidogrel, or certain antidepressants can be hit-or-miss without genetic testing. Even something as simple as smoking can boost CYP450 activity, forcing your doctor to adjust your dose.
What you’ll find in the posts below isn’t just theory—it’s real-world guidance. You’ll learn how to spot dangerous combinations, why your pharmacist asks about supplements, how food changes how your meds work, and what to do if a drug suddenly stops helping. From warfarin to melatonin to painkillers, these interactions shape whether your treatment works—or puts you at risk.